Diagnosis and the Triple Test
Assessment of Patient with Breast Symptoms
The Investigation of a Breast Symptom
Each year in Australia there are more than 400,000 general practitioner consultations to investigate breast symptoms. Although the majority of women who present with a breast problem will not have breast cancer, many women will experience significant anxiety associated with the development of a breast symptom. Women understandably often worry that their breast change is cancer. Although the changes we investigate may be uncomfortable or worrying to women, they are actually uncommonly cancer. There are many reasons for breast changes, and most are not dangerous or harmful. The prevalence of breast cancer in women with breast symptoms is in fact between 2 and 10%. All new breast symptoms and clinical abnormalities however must be appropriately investigated in order to exclude cancer.
The ‘triple test’ approach, the combination of clinical examination, breast imaging and nonsurgical biopsy is essential to maximise accurate diagnosis. Interpretation of the triple test result is critical; if there is any inconsistency, or all three parts of the triple test are not definitely benign, further assessment is required.
What investigations will the doctor suggest?
It is recommended that doctors use this approach known as the “triple test” to establish the cause of breast changes. It should be noted however, that many women with breast changes will not need all of these tests.
The Triple Test Approach to Diagnosis
The triple test refers to three diagnostic components:
- medical history and clinical breast examination
- imaging – mammography and/or ultrasound (+/-MRI)
- non-excisional biopsy – fine needle aspiration (FNA) cytology and/or core biopsy. This is when a sample of cells or tissue is extracted from the lump.
The sensitivity of the ‘triple test’ is greater than any of the individual components alone. The triple test is positive if any component is indeterminate, suspicious or malignant.
It is the responsibility of the managing clinician to correlate the pathological results with the clinical and imaging findings. Most women show no signs of cancer on any of the tests. The small number who do show possible signs of concern on one or more of the tests will be advised to undergo further investigations. The triple test is preferably managed by a single clinician who takes responsibility for coordinating the entire investigative pathway, and correlating the results with the woman’s symptoms.
Patient History and Clinical Examination
A history and clinical examination provide important information on which to base further investigation.
Patient history
Relevant history includes details of:
- current medications or recent changes, especially hormones such as the pill / HRT
- hormonal status /menstrual history
- previous breast problems, particularly previous breast investigations, biopsy results
- risk factors, particularly strong family history of breast /ovarian cancer.
- previous/ recent imaging /date and results /screening or diagnostic.
History of presenting symptom
- site — constant or changing
- duration — when and how first noted
- any changes since first noted
- relationship to menstrual cycles or exogenous hormones
- associated symptoms.
Clinical Breast Examination
After the woman has removed all clothing from the upper half of her body, the doctor will look at her breasts while she is seated to see whether any changes are visible. Following this, she will be asked to lie down, so the doctor can examine both breasts and nipples as well as the armpits.
The physical examination should establish the nature and site of any abnormalities found either on visual inspection or palpation of the breast. In particular, the physical examination should establish whether there is a discrete lump present or an area of textural change. The findings of the clinical examination should be correlated with the area of concern found by the patient or referring doctor, and also specifically with any abnormalities which may have been reported on imaging.

Diagnostic Imaging
The distinction between diagnostic breast imaging for the assessment of breast symptoms and breast screening is an important one. Screening is an assessment for women who have no breast symptoms. These women are being assessed, usually using mammography alone, with the aim of detecting breast cancer at an early stage. Women with breast symptoms should be advised not to attend Breastscreen Victoria for mammography, but are most appropriately assessed at a diagnostic imaging facility, often using both mammography and ultrasound, to provide an explanation for their symptoms and exclude breast cancer as a cause.
The sensitivity of mammography increases with increasing age. Sensitivity is improved with the addition of ultrasound over all ages though the size of this benefit is greater in women under the age of 50 years. Given the limitations of both mammography and ultrasound, they are often used in a complementary capacity to give information in the evaluation of breast abnormalities. Mammography and ultrasound used in combination will correctly identify about 95% of breast cancers in symptomatic women. Therefore, a small but significant proportion of breast cancers will not be diagnosed on imaging alone and clinical opinion is crucial in determining whether further testing such as biopsy is needed, despite normal imaging findings.
Mammography
Mammography is a low dose x-ray of your breasts. The use of breast x-rays sometimes causes people to be concerned about the amount of radiation used for the procedure, however mammograms only require a very low dose of radiation (which is similar to that which a person receives by flying from Australia to London and back).
A female mammographer (an expert in taking breast x-rays) will ask you to undress to the waist and stand in front of the mammography machine. If you are pregnant or think you may be pregnant, you should tell the mammographer. The breast is rested on the x-ray machine before it is gently but firmly compressed by a perspex plate so that all the breast tissue can be seen. Two or more images of each breast will usually be taken so that the breast tissue can be viewed from different angles.
Some women find having a mammogram quite uncomfortable or describe it as painful, but it only lasts a few seconds and it doesn’t cause any harm to the breasts. The breast is compressed in order to keep it still and get a clear picture. The test itself may take only a few minutes to perform, but you may be asked to wait a short time while the films are developed to check that the images are technically satisfactory and if additional views are needed. Further mammograms at different angles or with magnification are sometimes required to examine particular areas of the breast in greater detail.

Women with breast implants can still have mammograms. It is important to inform the mammography facility about breast implants when scheduling a mammogram. If the technician performing the procedure is aware a woman has breast implants, steps will be taken to make sure that as much breast tissue as possible can be seen on the mammogram.
Mammography should be performed in all age groups if the clinical or ultrasound findings are suspicious or malignant.

Breast Ultrasound
Unlike an x-ray, an ultrasound scan uses high-frequency sound waves to produce an image of the breast tissue. This is similar to the type of imaging technique used to scan babies in the mother’s womb during pregnancy. An ultrasound scan is painless and, while the length of time it will take varies, it can generally be done in a few minutes. You will be asked to undress to the waist and lie on a couch with your arm above your head. To help gain a clear image of the breast, some lubricating gel will be spread over the area of your breast to be imaged and the sonographer will use a hand-held scanning probe (called a transducer) which will be moved over the breast to look at the underlying breast tissue.
Regardless of age, an ultrasound scan will usually be done in addition to mammograms. An ultrasound scan does not provide the same information as a mammogram image. Both are often used in conjunction as they provide different information.


Ultrasound is:
- the breast imaging test of choice for young women (under 35 years) and women who are pregnant or lactating
- Useful in the evaluation of a specific lump or lesion in women of any age
- Very accurate when clinically guided or directed to an identified abnormality
- Highly operator dependent
- Preferred over mammography for image guided intervention such as biopsy and hookwire localisation if possible because it:
- avoids radiation
- allows ‘real time’ visualisation of needle or wire tip in relation to lesion
- avoids compression of the breast and is more comfortable for the patient
- is usually a quicker procedure than mammographic intervention procedures
Breast MRI
Breast MRI is an imaging technique that uses a magnetic field to create an image of the breast tissue. Unlike a mammogram, it does not involve any radiation exposure.
When you have a breast MRI, you will lie on a bed face down. You will go through a tunnel as the images are taken. Your breasts hang into special devices called breast coils, which improve the quality of the images. Your breasts are not compressed during an MRI (as they are in a mammogram). Hundreds of images are taken very quickly, and are stored in a computer for later analysis. It normally takes about 30 to 45 minutes to complete the scan. Usually an injection is given into a vein in your arm, and images are taken before and after the injection.
This injection helps to highlight blood flow in the breast. This helps the radiologist decide if a change in the breast is cancerous or not.


Magnetic resonance imaging is not recommended as a diagnostic test in women at average risk. Women with symptoms and/or image detected lesions should be assessed with the traditional triple test approach of clinical examination, imaging (mammography and/or ultrasound) and percutaneous biopsy and there is no role for MRI as a work up test for women with breast symptoms, except in very specific and uncommon clinical scenarios.
There is however, an increasing level of awareness of breast MRI among women presenting to their general practitioners and also to specialists with breast symptoms. It needs to be reinforced that in the context of the investigation and diagnosis of breast symptoms, MRI should be used only very selectively, in a problem solving capacity.
The cost of breast MRI is only covered by Medicare for screening women at potentially high risk of breast cancer by virtue of a strong family history, and there are very strict eligibility criteria about who can qualify for a Medicare rebate. There is currently no Medicare rebate for breast MRI used for women with breast symptoms.
Practice Tips
Under age 35
- Ultrasound is recommended as the first imaging modality.
- Mammography is usually only recommended if the clinical or ultrasound findings are suspicious or malignant, or on occasions if there is a strong family history of breast cancer.
35–50 years
- In keeping with expert consensus opinion mammography and targeted ultrasound are used
- as complementary modalities for the evaluation of symptomatic women in this age group
Over 50 years
- Mammography is recommended as the first imaging modality.
- Ultrasound is an acceptable initial investigation if:
- the lump is clinically consistent with a simple cyst and a normal (non-cancerous) mammogram has been performed in the last year. If the ultrasound does not confirm a typical cyst, further investigation including mammography must be performed.
- Ultrasound should also be used in addition to mammography:
- to help characterise mammographic abnormalities.
- if there is a clinical abnormality and either the mammogram is normal or the mammogram is unhelpful, eg extensive dense parenchyma
Ultrasound may be used in addition to mammography:
- to guide a fine needle aspiration or core biopsy
In pregnancy or lactation
- Ultrasound is the most useful modality
- Mammography should be used (with appropriate shielding) if the clinical or ultrasound findings are indeterminate, suspicious or malignant or there is inconsistency between test results.
Non Excisional Percutaneous Biopsy
Both fine needle aspiration (FNA) cytology and core biopsy have been shown to have high
specificity and sensitivity when used for palpable and impalpable lesions.
In a fine needle aspiration biopsy (FNA), a small sample of cells is drawn by a thin needle from the lump or area of breast change. This can be uncomfortable but rarely requires local anaesthetic. If the lump cannot be easily felt, ultrasound or mammography will be used to help the doctor guide the needle into the right area of the breast.


Fine Needle Aspiration (FNA)
A core biopsy is similar to a fine needle aspiration biopsy, except that a larger needle is used. Under a local anaesthetic, a very small cut is made in the woman’s skin and several samples of tissue are removed from the lump through the same cut using a spring loaded core biopsy device. Core biopsy provides a piece of breast tissue rather than just individual cells often making it easier for the pathologist to identify any changes.



Core biopsy device, needle and sample
- There are no absolute rules determining when FNA cytology or core biopsy is the more appropriate investigation.
- FNA cytology and core biopsy are complementary, although one may be more appropriate in achieving a definitive diagnosis. Core biopsy can often demonstrate invasive disease whereas FNA cannot differentiate between in situ and invasive cancer. Core biopsy can be used when FNA cytology fails to correlate with clinical findings or imaging studies
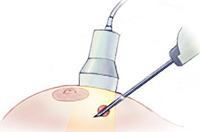
Needle biopsies (either FNA or core biopsy) may be performed freehand by the breast surgeon if the lesion is palpable, or under image guidance. Ultrasound is the preferred modality for image guided biopsy (pictured below) if possible because this is usually a quicker and simpler procedure than mammographic intervention procedures, and involves no radiation.
Lesions seen on mammography that require biopsy and cannot be felt or visualised using an ultrasound scanner, undergo biopsy performed on a special mammographic x-ray machine allowing three dimensional computerised images of the lump to be taken and used to guide the biopsy needle into the lump. This is called a Stereotactic Core Biopsy.

How accurate is the triple test?
If used on their own, none of the tests will be able to find all cancers. However, if all tests are done and none show signs of cancer, it is very unlikely that cancer will be present. If all three tests are performed, more than 99.6% of cancers will be found by one or more of the tests.

The sensitivity or true positive rate of the triple test is 99.6%. That means that in women who have breast cancer, the triple test will detect that cancer in 99.6% of cases. The specificity of the triple test is 62%. That means that in women who have no cancer, you will get a normal result in 62% of cases. This gives a false positive rate of 38%. That means that in women who have no cancer, the triple test will be positive in 38% of cases. This is because we include those classified as ‘indeterminate/equivocal’ in any one of the three components of the test as a positive outcome. For a test to be reliable in detecting an abnormality, you need a high sensitivity and thus the false positive rate will be high.
The sensitivity of needle biopsy is 90%, which may seem lower than expected. This is largely due to sampling techniques ie the lesion is not accurately targeted/sampled on FNA or core biopsy. It is vital that the results from biopsy correlate with both the clinical and imaging findings. If this is done, the sensitivity increases to >99.6%.
Implications for practice
Further investiagtion is recommended, in any of the following situations:
- where any one component of the triple test is positive i.e:
- clinical examination (suspicious or malignant)
- imaging (indeterminate, suspicious or malignant)
- FNA cytology or core biopsy (indeterminate, suspicious or malignant )
The Triple Test is the recommended approach to maximise diagnostic accuracy in the
investigation of breast changes.
- A triple test positive (indeterminate, suspicious or malignant) is found in 99.6% of
breast cancers. Any positive result requires further investigation, with the likelihood of cancer increasing if more than one component is positive. - A triple test negative on all components provides good evidence that cancer is unlikely
(less than 1%) and further investigation can be avoided for most of these women. - A small but significant proportion of breast cancers will not be diagnosed on imaging alone. Therefore, biopsy may be needed, despite normal imaging findings
- The triple test is preferably managed by a single clinician who takes responsibility for coordinating the entire investigative pathway, and correlating the results with the woman’s symptoms.

Open surgical biopsy
Usually, the ‘triple test’ gives enough information for the breast surgeon to be confident that a breast change is not cancerous. Sometimes however the surgeon or radiologist has a feeling that there is something about the lump that might not be normal, or some abnormalities may have been seen by the pathologist on FNA or core biopsy, that are felt to require further pursuit. The triple test requires a multidisciplinary approach and patients in whom there is discordance in the results of the components of the triple test will often be reviewed in our weekly Epworth Multidisciplinary Meeting. Sometimes, the consensus opinion will be that the only reliable way of excluding the presence of cancer is to proceed with an open surgical biopsy. In the past, prior to the advent of percutaneous needle biopsies, all breast lumps were subjected to open biopsy, however these days only a very small proportion will require removal specifically for diagnostic purposes.
An open surgical biopsy is a way of checking the whole lump/area for cancerous cells, rather than just a part of it. This test is used to provide the most accurate information about whether a cancer is present or not. An open biopsy is usually performed at a hospital as day surgery under a general anaesthetic.

If your breast lump is not easily felt or the abnormality is not a “lump” but something that has been detected only on imaging, its position in the breast might need to be marked with a fine piece of wire. A radiologist does this in the radiology department before the operation. Local anaesthetic is used to numb the skin. The wire is then inserted through a needle guided by a mammogram or ultrasound. The procedure is called a “hook wire localisation”. Some breast surgeons like Jane O’Brien, who use ultrasound themselves, can localise the area in question if it is visible on ultrasound in the operating theatre once the patient is asleep, using their portable ultrasound machine (pictured below) avoiding the need for the patient to undergo preoperative hookwire insertion.


Summary
The Triple Test is the recommended approach to maximise diagnostic accuracy in the
investigation of breast changes.
- The assessment of breast symptoms using the triple test requires a multidisciplinary approach.
- Each component of the triple test plays a part in revealing the likelihood of breast cancer or other diagnoses.
- The key to the triple test is the review of all results and correlation with the presenting symptom. If results are inconsistent or if they are benign but do not account for symptoms then further investigation is warranted.
- The correlation of findings of the triple test provides a sensitivity of nearly 100% in the detection of breast cancer.
- One clinician must take overall responsibility for correlating and interpreting the results of the clinical examination, the medical imaging and the pathology.
You will need the Adobe Reader to view and print these documents.
![]()











