Breast Cancer Recurrence

Although for many women undergoing surgery for early breast cancer the outlook is excellent, with an average 5 year survival of 91% in Australia, it is essential that ALL patients with invasive breast cancer are made aware of the possibility of subsequent
breast cancer recurrence.
I emphasise to all of my patients, that whilst to the best of my knowledge, the surgery has removed all traces of their breast cancer, and as such they can be currently regarded as “cancer free”, this alone cannot unfortunately always guarantee that a
recurrence won’t occur down the track sometime, and the reason therefore that other treatments in addition to surgery are considered /recommended, is in order to reduce to a minimum the chance of subsequent recurrence.
It is equally important that patients realise that additional “adjuvant” treatments, whether they be “systemic”, such as chemotherapy and hormonal therapies, which treat the whole body, and primarily aim to reduce the risk of “distant”
recurrence by eliminating clinically undetectable micrometastatic disease, or “local”, such as radiation, which primarily aims to reduce the risk of “local “ recurrence, also cannot be guaranteed to completely eliminate the
chance of recurrence, but will act to reduce that risk.
How Does Breast Cancer Spread?
Breast cancer can spread through the lymphatic system, the bloodstream, or uncommonly, by local invasion—which is when cancer cells actually invade nearby tissues, such as the chest wall or ribs.
When breast cancers spread and enter the lymphatic system, they usually first arrive at nearby lymph nodes and may still be early-stage. The spread of breast cancer to lymph nodes does
not necessarily mean that it’s “metastatic,” even though pathology reports often somewhat confusingly state “breast cancer metastatic to lymph nodes.”

A growing cancer may shed a cell or a clump of cells, and It can use your blood or lymph system as a network of highways for traveling. So, if a loose cancer cell makes it via the lymphatic system to your lymph nodes, it’s also possible that it may
spread via the bloodstream to other parts of your body.
When cancer recurs in a lymph node near the breast, it is considered a regional recurrence and not a distant recurrence.
When breast cancer spreads to lymph nodes it has essentially declared its intent to metastasize. Breast cancer reaching the lymph nodes is in effect a declaration that it’s working to spread further.
The lymph node evaluation, however, doesn’t give us a perfect answer either. Positive lymph nodes don’t necessarily mean that there are microscopic cells elsewhere with the ability to grow. In fact, they don’t in about 30 percent of
cases. Conversely, even if the lymph nodes are negative, it does not mean that the cancer has not spread—20 to 30 percent of breast cancers with negative lymph nodes have spread elsewhere.
To a certain degree, though, the number of positive lymph nodes gives us a sense of the probability of having microscopic breast cancer cells elsewhere in the body. With one or two positive nodes, you’re less likely to have the metastatic potential
than with ten or fifteen. However, because with any positive lymph nodes there’s a higher chance that there are cancer cells elsewhere that are capable of growing than with node negative breast cancers, we are more likely to treat women with
positive nodes with chemotherapy.
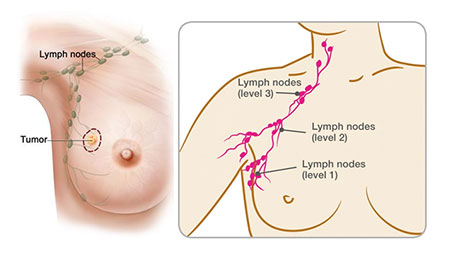
In women with negative nodes, it’s trickier. What we want is a way to identify the 20 to 30 percent who have microscopic cells elsewhere and not over-treat the other 70 percent. At present we don’t have a perfect way to do this.
The reason for adjuvant or neoadjuvant systemic therapy is the fact that breast cancer deaths rarely occur because of what is in the breast. You could have a lump as big as a basketball, and it would not kill you. What kills people with breast cancer
are the breast cancer cells that are in other, more important parts of the body, such as the lungs, liver, bone, or brain.
Metastatic or Secondary breast cancer is often referred to as “Stage 4” breast cancer and is considered the most advanced stage. It refers to breast cancers that have spread beyond the breast and nearby lymph nodes
to other regions of the body, which are called distant metastases.
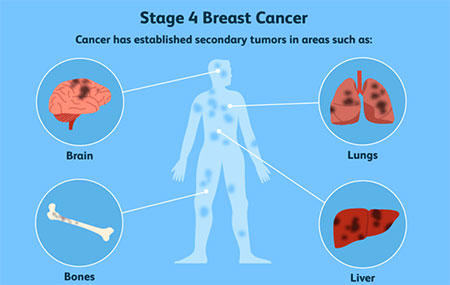
When breast cancer spreads it is still breast cancer. If you were to take a sample of the cancer in these locations and look at it under the microscope, the appearance would be of cancerous breast cells, not bone, liver, or lung cells. Thus,
for example, breast cancer that has spread to the bones is not called bone cancer, but rather “breast cancer metastatic to the bones.”
What is a breast cancer recurrence?
Breast cancer recurrence means that the cancer was diagnosed when limited to the breast and/or armpit lymph nodes, then treated, and at some time later has come back.

This can occur in several ways:
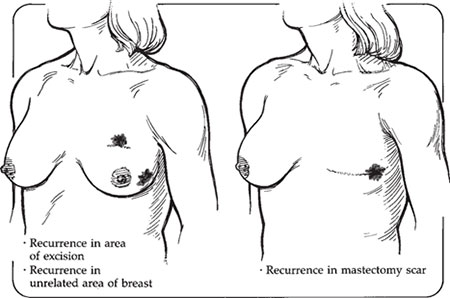
- Local and/or regional recurrence: the breast cancer that was previously treated returns within the breast, chest wall or regional lymph nodes.
- New primary breast cancer: an unrelated new breast cancer occurs in one or the other breast. This actually isn’t a local recurrence at all—it’s a new cancer in the breast (often referred to as a new primary). This typically occurs
many years after the original cancer and in an entirely different area of the breast. Its pathology is often different —lobular instead of ductal, for example. Though they are often counted as recurrences in the statistics for breast conservation,
they should be treated as completely new cancers, much as with new cancers in the opposite breast. - Distant or systemic recurrence or metastasis is much more serious than local recurrence and is synonymous with stage 4 disease. For breast cancer patients, the most common areas of spread are the bone, liver, lungs and brain
Breast cancer recurrence occurs if:
- Cells from the original breast cancer diagnosis break away and hide nearby in the breast (called local recurrence) or spread elsewhere in the body (called distant recurrence);
AND
- Treatment, including surgery, chemotherapy, radiotherapy and/or hormone therapy have not gotten rid of all these cancer cells from the body.
These cells can begin to grow right away or can remain dormant for many years before beginning to grow and travel further through the body.
Many recurrences are detected in the five years after diagnosis, especially after triple negative breast cancer. However, on occasions recurrence can occur more than 20 years after the first diagnosis.
Breast cancer survivors are at risk for developing new cancers for a number of reasons – whatever caused the original cancer could still be having an effect, either on second primaries in the same organ, or on related cancers in other organs. This can
be due to genetic predisposition, as is sometimes the case with breast cancer .
Your individual chance of breast cancer returning is also determinate on a number of factors including the type of breast cancer, tumour size, genetic factors and treatment types.
How does distant recurrence occur?
Many patients find it hard to understand how they can be apparently “cancer free” one day and be diagnosed with recurrent cancer the next. If surgery got all of the cancer out and chemotherapy and radiation were supposed to have mopped up
the rest, how can recurrence even happen?

In most cases, even the smallest breast cancer detected has been growing for some time before it was caught. During this period of growth, the cancer cells multiplied and divided over and over again, and some cancer cells may splinter off from the main
tumour and escaped into the surrounding blood and lymphatic vessels. Cells that spread to lymph nodes can certainly be trapped in those lymph nodes and removed at the time of surgery, but cells can also go into the circulatory system. Even early-stage
cancers that originally had no lymph node involvement can recur and develop metastatic disease.
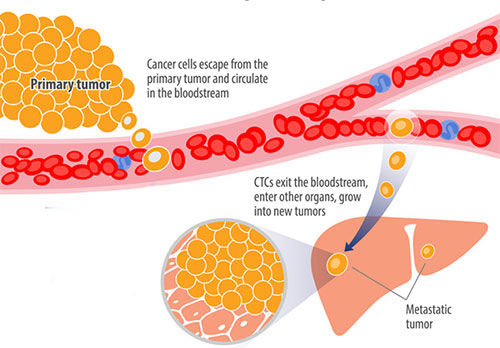
While it’s less common, cancer cells can bypass lymphatics and lymph nodes and travel via surrounding blood vessels. Cancer cells can continue to circulate and go anywhere the blood vessels will take them, or they can home in on other organs in
the body, where they take up residence and continue to grow and divide in that one particular spot.
If and when cancer comes back, the cancer cells that escaped the breast are to blame. Obviously if your recurrence is ten years after your diagnosis, we assume that the cells have been dormant (sleeping) all that time and missed the treatments aimed at
dividing cells.
Why weren’t these escaping cells identified the first time the cancer was treated?
Although scans of the body can detect if there is obvious spread to these other organs, for women with early stage breast cancer there rarely is anything that shows up on a scan. There is a limit to what scans can tell us: they won’t show
extremely tiny spots of cancer, and they definitely can’t show us if there are individual cells circulating in the body. Neither will any blood test, or any other test for that matter. So the first time around we perform our surgery and give
our treatments—chemotherapy, hormonal therapy, radiation—with the hope that if microscopic spread has already taken place, the treatments will scavenge those cells and kill them before they take up residence someplace in the body.
Unfortunately, these treatments don’t work 100 percent of the time. So if cells have spread, and if the treatments we give don’t affect them, the cancer cells can persist and take hold someplace, developing into metastases,
or spread. This is why and how recurrence happens.
If all the cancer was removed with surgery, why do I need any additional treatment ?
It has long been recognized that breast cancer is not always cured by locoregional treatment alone.
The goal of treating early breast cancer is to remove the cancer and keep it from coming back (breast cancer recurrence). Most people diagnosed with breast cancer will never have a breast cancer recurrence. However, everyone who has had breast cancer
is at potential risk of recurrence, and that is why in most cases, there is a recommendation for treatment in addition to surgery, which is known as “adjuvant” therapy. The risk of recurrence can never be entirely eliminated, but
the aim of adjuvant therapy is to reduce recurrence risk to the absolute minimum.

Who Is at Risk of Breast Cancer Recurrence?
Everyone who has received a breast cancer diagnosis is at risk of recurrence, however the risk differs markedly depending on a number of factors listed below. Some breast cancers, when diagnosed very early when small and without lymph node involvement,
have an excellent prognosis and are very unlikely to recur. On the contrary, larger cancers, with lymph node involvement or with a more invasive behaviour, are unfortunately at a higher risk of recurrence.
What is my prognosis?
This is a very common question that isn’t always easy to answer. There are many factors involved in working out prognosis. Remember that a prognosis is just a figure at the point at which you receive it. For most people, the prognosis gets better
with time.
Sometimes we use a five-year figure because we know that if cancer comes back, most of the time it comes back within five years. If the cancer has not come back within five years, then the chance of it coming back within ten years is quite low, and if
it does not come back within ten years, then you have an almost normal life expectancy.
It’s a bit like buying a second hand car. You don’t really know how long it’s going to last, but if it lasts year after year without breaking down, then the car starts to look more and more reliable to make that long trip.
Working out prognosis can be difficult.
How is a local recurrence after lumpectomy diagnosed?
After a diagnosis of early stage breast cancer, any remaining breast tissue should be evaluated annually with scans (such as mammogram or ultrasound).
Most local recurrences within the breast after lumpectomy are detected on routine annual breast imaging, which usually takes the form of mammography and ultrasound, and on occasions MRI.
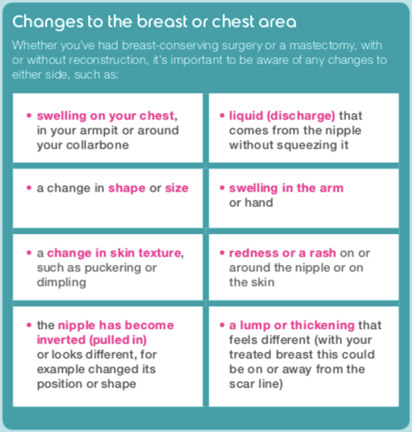
If you have a local recurrence or new primary breast cancer, you may find symptoms similar to an initial breast cancer. This includes:
- A new lump in the breast, armpit area or around the collarbone
- A change in breast size or shape
- Changes to the nipple, such as sores or crusting, an ulcer or inverted nipple
- Clear or bloody nipple discharge
- Changes to the skin including redness, puckering or dimpling (an ‘orange peel’ appearance)
- Breast tenderness or pain
Once a local recurrence has been diagnosed, we do tests to see whether there are signs of cancer elsewhere in the body. These may include a chest X-ray, CT scan, bone scan or PET scan, and blood tests (some of the latter are looking for tumour markers.
If the tests are normal (only 5 to 10 percent of women with local recurrence following lumpectomy have signs of disease elsewhere), then we have to figure out how best to treat the tumour in the breast. Usually in these cases we do a mastectomy, as
the prior less drastic surgery and radiation didn’t take care of it.
Am I Still at Risk of local Recurrence if I Have Had A Mastectomy?
Yes. Local recurrence can also happen after a mastectomy, although the likelihood is usually low.
Some of the signs of local recurrence after mastectomy include
- A lump or raised bump in or under the skin, especially near the previous mastectomy scar
- Changes to the skin, including redness or thickening

After reconstruction a local recurrence can appear at the suture line of the flap or in front of the implant. When it’s in the skin itself, it is red and raised. Reconstruction rarely if ever hides a recurrence. With implants, the recurrences are
in front of the implant. With a flap, the recurrences are not in the flap itself (tissue from the abdomen) but along the edge of the breast skin.
Local recurrence after mastectomy is often described as a “chest wall” recurrence, which isn’t entirely accurate because it implies that the cancer is in the muscle or bone. But usually such a recurrence appears in the skin and fat where
the breast was before, and only rarely does it include the muscle.
Ninety percent of local recurrences following mastectomy happen within the first five years after the mastectomy. Approximately 20 to 30 percent of women with local recurrences after mastectomy have already been diagnosed with metastatic disease, and
another 20 to 30 percent will develop it within a few months of diagnosis. Therefore, just as with local recurrences after breast conservation, tests should be done to look for distant disease.
How are local and regional recurrences treated?
The treatments for local recurrences are also primarily “local”. Local and regional recurrences may feel just as devastating as distant disease, but depending on the circumstances, they may represent a different situation with a somewhat better
prognosis.
Treatment of local recurrence after previous lumpectomy
Mastectomy
Recurrence in the same breast is treatable and potentially curable again.
However, mastectomy, with or without immediate reconstruction, is the recommended procedure the second time around (lumpectomy and radiation go together, and radiation is no longer an option, as it cannot be given to the same area twice)..
Treatment of local recurrence after previous mastectomy
Most commonly the lesion is removed surgically and followed by radiation to the chest wall if the woman has not previously had radiation Treatment of local recurrence after mastectomy can involve a variety of different approaches, including surgery to
remove the recurrence if it is confined to a limited area. Other options for treatment include radiation, chemotherapy, and endocrine therapy, or a combination of these.
Despite aggressive local treatment, many women with an isolated local recurrence following mastectomy eventually develop distant metastases. This is not because the local recurrence spreads, but rather because it is a sign that things have changed and
dormant cells in other organs may also be waking up.
Regional recurrence
Regional recurrence usually refers to cancer that has recurred in the usually the lymph nodes under your arm. In many cases treatment for regional recurrence, like local recurrence, can involve surgically removing the area of recurrence, but also can
involve radiation, chemotherapy, hormonal therapy, or some combination thereof.
As physicians, we tend to downplay local and regional recurrences because they are not as life threatening as metastatic disease can be. Nonetheless, for the patient, they can be devastating. When a woman gets a local recurrence, she finds it much harder
than she did the first time not to think of herself as doomed. She gave it her best shot and it didn’t work— how can she trust any treatment again?

The process of psychosocial adjustment starts all over again; learning to trust your body may take longer when you’ve been doubly betrayed by it. The feelings you experienced the first time around are intensified because now you not only don’t
trust your body but also begin to second guess your doctors and treatment in general. Should I have gone somewhere else for treatment? Was it the fact that I was too stressed? Should I have had a mastectomy or chemotherapy, exercised more or drank
that special tea my cousin told me about?
These are very common feelings, but it is important to remember that a recurrence is almost never your doctor’s fault or your fault; it’s the result of factors we do not understand and cannot control. And no matter how much you second guess
your treatment, you can’t change it now.

Where does breast cancer spread elsewhere in the body?
Secondary breast cancer is breast cancer that has spread from the breast to other parts of the body. Breast cancer starts in the breast – this is primary breast cancer. In many women, primary breast cancer does not come back after treatment. However, in some women, cancer cells break away from the primary breast cancer and spread to other parts of the body
through the bloodstream.
These cancer cells go on dividing and form a new cancer, known as a secondary cancer or metastasis.
The secondary cancer is made up of breast cancer cells. This means that, for example, a secondary breast cancer in the liver behaves as – and is treated as – breast cancer, not a primary liver cancer.
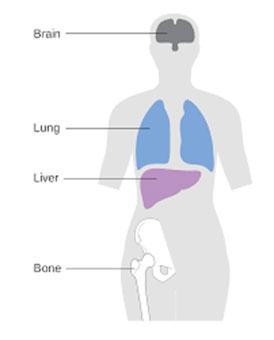
For breast cancer patients, the most common sites of distant spread are:
- Bones
- Lungs
- Liver
- Brain
- Peritoneal cavity (pelvis and abdomen)
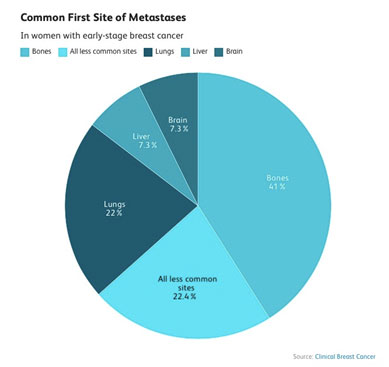
A 2013 study looked at the most common first site of metastases in women with early-stage breast cancer. The frequencies were:
- Bones: 41%
- Lungs: 22%
- Liver: 7.3%
- Brain: 7.3%
- All less common sites: 22.4%
For roughly a third of women cancer spreads to multiple organs at the same time.
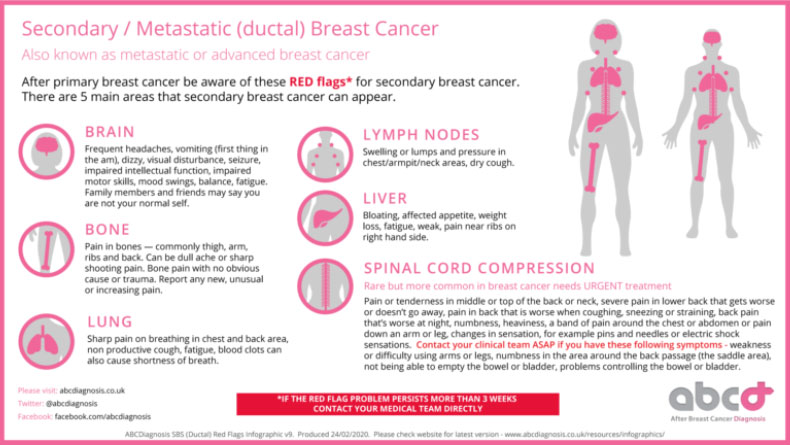
Reproduced from abcdiagnosis.co.uk
Invasive lobular carcinoma tends to have a different pattern of metastases than ductal breast cancer. In one 2017 study,
almost 70% of people with metastases from lobular carcinoma had peritoneal metastases.
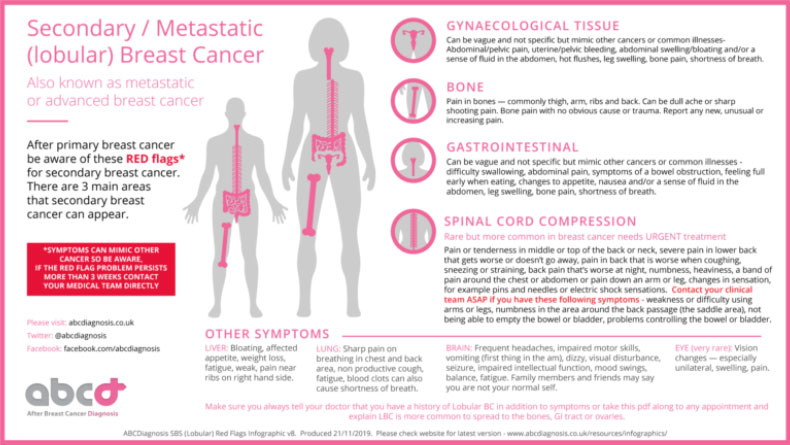
Reproduced from abcdiagnosis.co.uk
Risk Factors for Distant Recurrence
There are several risk factors that raise the risk of recurrence overall (combining both early and late recurrences). These include:
- Tumour size: Larger tumours are more likely to recur than smaller ones both early and late.
- Positive lymph nodes: Tumours that have spread to lymph nodes are more likely to recur at any time than those that
have not. - Age at diagnosis: Breast cancer recurrence is more common in younger women.
- Treatments received and response to treatments: Both chemotherapy and hormonal therapy (tamoxifen or aromatase inhibitors) reduce the risk of recurrence
- Tumour Characteristics: More aggressive cancers (grade 3) are more likely to recur than less aggressive tumours (for example, grade 1), especially in the first five years. We also take into account the receptor status (ER/PR/HER2)
and an estimate of proliferation (Ki67).
There are also factors that do not appear to affect the risk of recurrence. Recurrence rates are the same for women who have a mastectomy or lumpectomy with radiation and are also the same for women who have a single vs. double mastectomy.
What Are The Signs of distant Breast Cancer Recurrence?
If your breast cancer has spread to other parts to the body, known as distant recurrence, there are a number of possible symptoms, including:
- Fatigue
- Breathlessness
- Pain in your bones
- Unexpected weight loss or change in appetite
- Severe or ongoing headaches
- Nausea

However, symptoms will vary depending on where the secondary cancer presents. Sometimes recurrence is identified on a scan or blood test that was done for a reason other than breast cancer.
Studies have shown that doctors are sometimes reluctant to mention the symptoms of metastatic disease. In medical school it was suggested that we shouldn’t tell people who had been treated for cancer what to look for if they were worried about recurrences
because they’d start imagining that they had every symptom we told them about, but that doesn’t reassure people at all; it just means they’ll be afraid of everything instead of a few specific things. When you’ve had cancer,
you’re acutely aware of your body, and any symptom that’s new—or that you never noticed before—can take on terrifying significance as you worry that your cancer may be back. Inevitably this will mean a lot of fear over symptoms
that turn out to be harmless.
But if you know that the symptoms of breast cancer metastasis are usually bone pain, shortness of breath, lack of appetite and weight loss, and neurological symptoms like pain or weakness or headaches, there are at least limits to your fear. You’ll
probably be frightened when anything resembling those symptoms comes up, even if it turns out to be nothing but a tension headache or a mild flu. But at least you won’t be terrified by a sore spot on your big toe or an unexpected weight gain.
Knowing what symptoms to look for reduces fear; it doesn’t increase it.
As hard as it is to face a local recurrence, metastatic disease can be even more devastating. It causes the same feelings that go with any recurrence, compounded by the knowledge that the chance of permanent cure is low. Contrary to common belief, metastatic
breast cancer is rarely an immediate death sentence, and these days, with good treatment, women with metastatic breast cancer often live for a number of years with a reasonably good quality of life.
The prognosis for metastatic disease depends on which molecular subtype your tumour or recurrence belongs to. Women with hormone- positive breast cancers tend to have recurrences much later than those with hormone-negative ones. This may be in part because
they take hormone therapy for five to ten years that may keep things under control and also because these cancers tend to be less aggressive. They also tend to respond better to treatments for their metastatic disease. HER-2 positive tumours used
to be the most aggressive, but now, with the use of Herceptin at the time of diagnosis and new anti HER-2 drugs at the time of recurrence, they have a much better outcome. And even the women with triple-negative metastatic disease, who generally have
the worst prognosis, can use a menu of new and old drugs to keep the tumour guessing for a couple of years. Finally, though not to be too optimistic, new drugs such as immunotherapy are changing the scene.
When cancer does recur elsewhere in the body, it can take many courses. Some women with recurrence can live for many years taking medication that keeps the cancer at bay. Some women have a more rapidly declining course, where none of the many medications
and treatments we have to offer seem to work. And while there is always room for optimism, there is no doubt that anytime cancer returns this is a devastating scenario for patients and their families.
As I explain to my patients, there are good reasons these days to remain optimistic, even after cancer comes back. Newer, better treatments are becoming available all the time. And for women who were treated a long time ago, the options for treatment
may have changed and improved significantly since the first time they were treated
Should I have regular routine scans or blood tests to check for distant breast cancer recurrence?
No. Routine scans to check for the presence of distant disease recurrence are not recommended in the absence of symptoms
Given the ominous nature of stage 4 disease, the obvious question is, why don’t we scan for spread regularly after a first diagnosis, so that we can detect it early if it does return? The reason we don’t scan or test for metastasis is that
there really is no “early” stage 4 disease, and thus no real opportunity to intervene earlier and increase the chance of cure. It’s also important to know that with recurrence, one does not progress from one stage to the next: a
woman who was originally diagnosed with stage 1 breast cancer does not recur as stage 2, because once cells have taken up residence elsewhere, she is immediately considered to have stage 4 disease. And with stage 4 disease, either you respond well
to treatment and the disease regresses, or you don’t and it doesn’t. Studies have shown that getting frequent scans after a first cancer diagnosis does not lead to improved survival, which is why we don’t scan for stage 4—even
if we wish we could.
Current guidelines and evidence therefore recommend against routine CT or bone scans, or blood tests, to look for recurrence of cancer in patients who do not have any symptoms or other concerns that need to be followed up on.
If you do have concerning symptoms (such as those mentioned above), then you should bring them to the attention of your healthcare team to be checked out.
Am I more likely to experience a distant recurrence if I have had a lumpectomy compared to a mastectomy?
No. The nature of the surgery to your breast has NO influence on the chance of the breast cancer recurring distantly in other organs.
Some women with recurrence can live for many years taking medication that keeps the cancer at bay. Some women have a more rapidly declining course, where none of the many medications and treatments we have to offer seem to work. And while there is always
room for optimism, there is no doubt that anytime cancer returns this is a devastating scenario for patients and their families.
How long after breast cancer treatment do recurrences occur?
The risk of recurrence for all breast cancers was highest in the first five years from the initial cancer diagnosis at 10.4%. This was highest between the first and second years after the initial diagnosis. During the first five years after the initial
diagnosis, patients with oestrogen receptor (ER) positive breast cancer had lower rates of recurrence compared with those with ER negative disease. However, beyond five years, patients with ER positive disease had higher rates of recurrence.
The “late recurrence” or relapse of breast cancer refers to cancers that come back after five years, but may not return for 10 years, 20 years, or even more. For people who have estrogen receptor-positive tumours, the cancer is actually more likely
to recur after five years than in the first five years.
In contrast to the common belief that surviving for five years after cancer treatment is equivalent to a cure, with hormone-sensitive (estrogen and/or progesterone receptor-positive) breast tumours there is a steady rate of recurrence risk for at least 20
years after the original diagnosis, even with very small node-negative tumours.
An awareness of the risk of late recurrence is important for a number of reasons. People are often shocked to learn that their breast cancer has come back after say, 15 years, and loved ones who don’t understand this risk are often less likely to be supportive
as you cope with the fear of recurrence.
While chemotherapy has little effect on the risk of late recurrence hormonal therapy does, and estimating this risk may help determine who should receive extended hormonal therapy (beyond five years). Finally, late recurrences can differ from early relapse
(within five years) with regard to sites of metastases and survival.
Factors such as initial tumour size, number of nodes involved, and receptor status play into the risk of late recurrence, but tumour biology appears to have the greatest effect, and research is actively looking for ways to look at gene expression and
copy number to predict risk.

When treating breast cancer that has metastasized to other parts of the body, the philosophy is usually to use the minimum amount of treatment needed in order to control the disease. Treating the disease aggressively does not improve survival, but it
does increase side effects and lessen the quality of life.
Bone Metastases
The most common site of distant breast cancer metastases, occurring in around 70% of people with metastatic breast cancer, is the bones. The ones most commonly affected include:
- Spine
- Ribs
- Pelvis
- The long bones of the arms and legs
Bone metastases tend to have a fairly good prognosis relative to metastases to some other regions of the body.

Symptoms and Detection
While bone metastasis may cause pain, that is not always the case. Some people are unaware that they have bone metastasis until they suffer a fracture from what should’ve been a minor trauma. Fractures through a portion of a bone weakened by cancer metastasis
are called pathologic fractures.
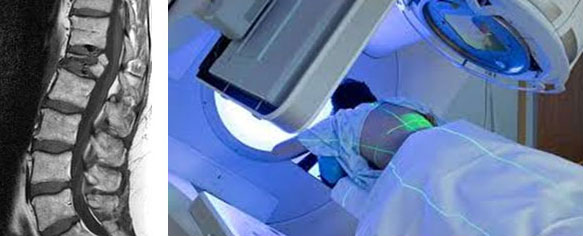
Treatment
Several types of treatment are available for bone metastases from breast cancer, and some of these can control the disease for quite some time.
- Radiation therapy is often done when rapid relief is needed, and it can be very effective for the local treatment of bone metastases.
- Sometimes surgery is needed to stabilize a bone that has fractured or is at risk of fracturing due to metastases. When bone metastases occur in the spine, they can sometimes lead to spinal cord compression, a condition that requires immediate attention to prevent paralysis and more.
- Bone-modifying medications are a newer treatment for bone metastases and can be very effective. Bisphosphonates such as Zometa (zoledronic acid) are not only effective in reducing pain from metastases but appear to have anti-cancer effects as well. These medications may also reduce the chance
of further bone metastases and improve survival. Denosumab may also be effective in treating bone metastases while improving survival.
Liver Metastases
Breast cancer metastases to the liver are also common.
Symptoms and Detection
Liver metastases may be present without any symptoms. If symptoms do occur, they can include:
- Abdominal pain
- Nausea
- Itching (which can be severe)
- Jaundice (a yellowish discoloration of the skin and the whites of the eyes)
Sometimes, liver metastases are suspected based on abnormal liver function tests.
Treatment
General treatments for metastatic cancer (such as chemotherapy, hormonal therapies, and targeted therapies) may decrease these
metastases, but since the liver acts as the detoxification centre of the body, treatments must be delicately balanced, as sometimes, liver metastases reduce the ability to tolerate chemotherapy.
Lung Metastases
Just as the blood is filtered by the liver, blood passes through the lungs, making this a common site of breast cancer metastasis.
Symptoms and Detection
The most common symptom of lung metastases is shortness of breath, which may be mild and only occur with exercise at first. Other symptoms can include a persistent cough or pain with breathing.

Lung metastases may be suspected based on a scan, which often shows multiple small areas of metastases (in contrast to lung cancer, for example, which is more likely to appear as a single large mass).
In addition to spreading to the lungs, metastatic breast cancer often causes pleural effusions—a build-up of fluid in the space between the membranes (the pleura), which line the lungs.
Treatment
Lung metastases are often treated by the general treatments for metastatic breast cancer, but radiation therapy may be helpful, especially if the metastases cause an obstruction in the airways (bronchi). If only a few metastases are present, treatment
to eradicate these may be considered.
Before treatment, however, it’s important to make sure that a nodule in the lung is, indeed, due to breast cancer. Primary lung cancer is treated differently than breast cancer that spreads to the lungs.
Pleural effusions can be quite large and cause significant shortness of breath. The fluid is often removed by placing a needle through the chest wall and into the pleural cavity to drain the fluid. Unfortunately, pleural effusions often recur. When this happens, a pleurodesis may be recommended (a procedure in which the layers of the pleura are scarred together so fluid cannot reaccumulate).
Brain Metastases
Breast cancer spreads to the brain in about 10% to 15% of people with metastatic breast cancer overall. Brain metastases are more common in women with HER2-positive tumours and triple-negative breast cancer, with brain metastases occurring in roughly
a third of people with HER2-positive breast cancers that metastasize.
Symptoms and Detection
Symptoms of brain metastases often include:
- Headaches
- Visual changes
- Dizziness
- Seizures (sometimes a seizure is the first symptom)

Other symptoms may include:
- Weakness on one side of the body
- Problems with coordination
- Personality changes
Not everyone with brain metastases has symptoms, though. Sometimes, they’re only found because of imaging tests performed on the brain.
Treatment
Unlike metastases to some other regions, treatments such as chemotherapy and targeted therapies are often ineffective against brain metastases due to the blood-brain barrier, which is a tight network of capillaries designed to protect the brain from toxins (such as chemotherapy).
The treatment of metastases usually includes steroids to decrease swelling in the brain. Surgery to remove a single or only a few metastases (called a metastasectomy) has been used in recent years and may improve survival when used for people who are
good candidates for the procedure.
Stereotactic radiotherapy uses a high dose of radiation to a small area of tissue to attempt to eradicate metastases. It is usually used when only a few metastases are present, but some centres have treated people with up to 10 metastases at a time. The
procedure can also be repeated to treat additional metastases which are present or which occur over time. Stereotactic radiotherapy can be a better option than surgery for metastases which are deep in the brain, or in sensitive regions where surgery
would cause too much damage to healthy brain tissue. It is most effective with small metastases, and surgery may be a better option for metastases greater than 3 cm in diameter. There is less cognitive decline seen with stereotactic radiotherapy than
with whole brain radiotherapy, although some side effects, such as radiation necrosis, may occur.
Whole-brain radiation may also be used to address the metastases.
Less Common Sites of Distant Metastases
Breast cancer can spread to nearly any region of the body. Some of the less common sites of metastasis include:
- Bone marrow
- Leptomeningeal Metastases
- Peritoneal metastases (accounting for two-thirds of people with metastatic lobular carcinoma)
- The opposite breast (v uncommon)
- An ovary
- Adrenal glands
- Pancreas
- Skin and soft tissue
Patient Information
![]() Guide For Women Secondary Breast Cancer
Guide For Women Secondary Breast Cancer
![]() Understanding Secondary Breast Cancer
Understanding Secondary Breast Cancer
![]() Clinical Carson Advanced Breast Cancer
Clinical Carson Advanced Breast Cancer
![]() Metastatic Breast Cancer: an introduction
Metastatic Breast Cancer: an introduction
![]() Secondary breast cancer Information pack
Secondary breast cancer Information pack
![]() Secondary breast cancer in the bone
Secondary breast cancer in the bone
![]() Secondary breast cancer in the liver
Secondary breast cancer in the liver
![]() Secondary breast cancer in the brain
Secondary breast cancer in the brain
![]() Secondary breast cancer in the lungs
Secondary breast cancer in the lungs
Advanced/Metastatic Breast Cancer Clinical Guidelines:
![]() Esmo Metastatic Guidelines 2021
Esmo Metastatic Guidelines 2021
![]() Ago Metastatic Guidelines 2020
Ago Metastatic Guidelines 2020
![]() ASCO Chemotherapy and Targeted Therapy for Metastatic
ASCO Chemotherapy and Targeted Therapy for Metastatic
References:
![]() Incidence and Patterns of Distant Metastases for Patients With Early-Stage Breast Cancer After Breast Conservation Treatment
Incidence and Patterns of Distant Metastases for Patients With Early-Stage Breast Cancer After Breast Conservation Treatment
![]() Annual Hazard Rates of Recurrence for Breast Cancer During 24 Years of Follow-Up
Annual Hazard Rates of Recurrence for Breast Cancer During 24 Years of Follow-Up
![]() 20-Year Risks of Breast-Cancer Recurrence after Stopping Endocrine Therapy at 5 Years
20-Year Risks of Breast-Cancer Recurrence after Stopping Endocrine Therapy at 5 Years
You will need the Adobe Reader to view and print these documents.
![]()











