Breast Cancer Clinical Guidelines
Breast Cancer Clinical Practice Guidelines, Consensus Documents and Position Statements
Over time, some areas of breast cancer management may go through a phase of rapid change, whilst others may remain relatively constant over that time. Changes may occur as a result of the introduction of newer drugs or operative techniques. Most significant changes in practice come about following randomised trial evidence demonstrating efficacy.
From the maximum tolerable to the minimum effective treatment, it is essential to escalate treatment when necessary, and to de-escalate when unnecessary. The most significant changes in breast cancer surgery and radiation oncology in the recent past involve “de-escalation”, the aim of which is to protect patients as much as possible from unnecessary morbidities of treatment, and to make treatment more tolerable.
For example, instead of the previous 25 or 30 fractions of postoperative radiation after surgery for early breast cancer, which was administered over 5-6 weeks, it is now fairly standard that “hypofractionated” radiation courses are recommended in most cases, which usually involve 16 fractions over around 3 weeks, which proves much more convenient for patients.
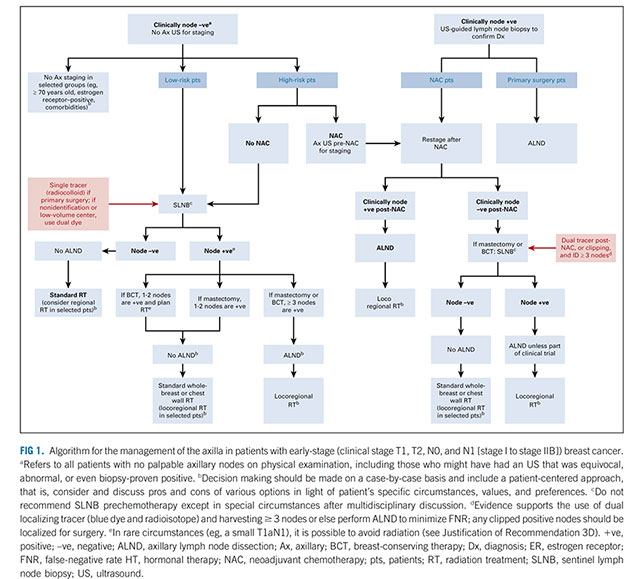
In breast cancer surgery, there is no benefit to patients in removing all the lymph nodes under the arm (axilla) if there is no tumour in any of the nodes, and performing an axillary node clearance in this circumstance exposes patients to potential long term sequelae such as lymphoedema, for no potential benefit. It is therefore standard that sentinel node biopsy is undertaken in women with unknown nodal status, both in the setting of primary surgery, and also following neoadjuvant chemotherapy. Similarly, in women who are node positive prior to neoadjuvant chemotherapy, particularly in cases of HER2+ or triple negative breast cancer, if there appears to have been a good response to neoadjuvant therapy, less than axillary node clearance is often recommended, with restaging of the axilla after treatment with sentinel node biopsy +/- targeted axillary dissection (TAD), which involves targeted removal of the node biopsied prior to neoadjuvant therapy.
Algorithm for the management of the axilla in patients with early-stage breast cancer ASCO 2021
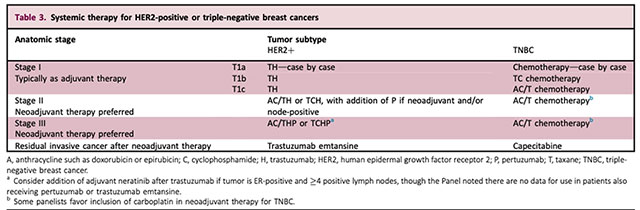
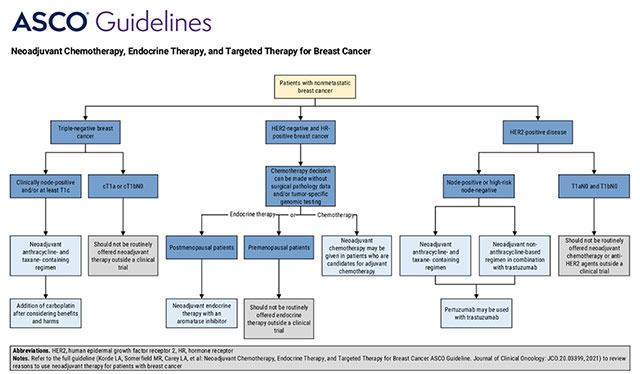
Traditional clinicopathological staging, taking into account the size and nodal status of the tumour, has become less influential than in the past in the development of systemic treatment recommendations, and with advances in the molecular classification of breast cancer, tumour biology is now a driving force. The treatment of HER2+ve breast cancer is for example, currently changing and evolving, with the high response rate to neoadjuvant therapy in HER2+ve disease, frequently allowing de-escalation of surgery in both the breast and axilla, at the same time as escalating systemic therapy, often with dual agent HER2 blockade with trastuzumab and pertuzumab, and the addition of postoperative, “adjuvant” trastuzumab emtansine for patients with residual invasive cancer breast cancers after neoadjuvant therapy.
Systemic therapy for HER2-positive or triple-negative breast cancers
St Gallen International Consensus Guidelines 2021
It is not practical for textbooks to be updated frequently enough to reflect current practice in all areas of breast cancer treatment, especially those that are in rapid evolution, and there are a range of practice documents that provide current, up to date information, including clinical guidelines, consensus documents and position statements.
Clinical practice guidelines, consensus documents and position statements are evidence-based or consensus-based documents developed to assist healthcare professionals and patients with decision-making related to screening, prevention and treatment of breast cancer, and to promote high quality and appropriate care. They are developed from the body of established literature complemented by expert opinion. A position statement provides a short summary of clinical issues in a specific area of practice and may be complemented by a clinical guideline. Clinical guidelines, are documents with the aim of guiding decisions and criteria regarding diagnosis, management, and treatment. They are based upon the best available research evidence and practice experience. They are developed by multidisciplinary committees or panels that follow a rigorous evidence-based approach, and are based on a systematic review of the available evidence, following transparent development and decision making processes. They are informed by the judgement of the evidence by experts, and the views of consumers and other people affected by the guidelines.
Clinical guidelines are developed for use by recognised health organisations such as colleges, professional societies or government. They have a limited life, and are reviewed for their currency and validity on a regular basis, and updated or withdrawn in light of important new evidence that may emerge. Because they are regularly updated, clinical guidelines, consensus documents and position statements provide the most up to date information on a given area of practice.
Below are breast cancer related practice documents for health professionals and patients from a variety of international organisations. For Advanced/Metastatic Breast Cancer Clinical Guidelines see Breast Cancer Recurrence.
United States
American Society of Clinical Oncology (ASCO)
- Exercise, Diet, and Weight Management During Cancer Treatment: ASCO Guideline (2022)
- Biomarkers for Adjuvant Endocrine and Chemotherapy in Early-Stage Breast Cancer – ASCO Guideline Update 2022
- Neoadjuvant Chemotherapy, Endocrine Therapy, and Targeted Therapy for Breast Cancer: ASCO Guideline (2021)
- Management of the Axilla in Early-Stage Breast Cancer: Ontario Health (Cancer Care Ontario) and ASCO Guideline (2021)
- Selection of Optimal Adjuvant Chemotherapy and Targeted Therapy for Early Breast Cancer: ASCO Guideline Update (2020)
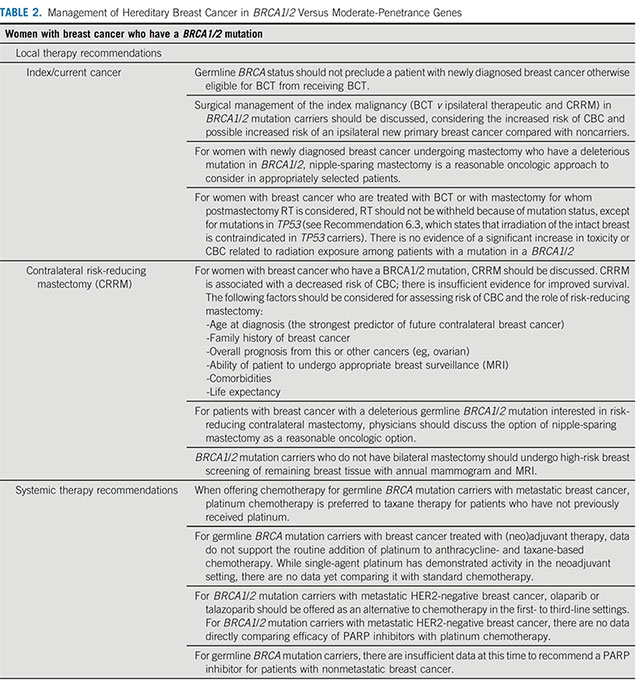
- Management of Hereditary Breast Cancer: American Society of Clinical Oncology, American Society for Radiation Oncology, and Society of Surgical Oncology Guideline (2020)
- Lumpectomy Margins for Invasive Breast Cancer and Ductal Carcinoma in Situ: Current Guideline Recommendations, Their Implications, and Impact (2020)
- Management of Male Breast Cancer: ASCO Guideline (2020)
- Prevention and Management of Chemotherapy-Induced Peripheral Neuropathy in Survivors of Adult Cancers: ASCO Guideline Update (2020)
- Estrogen and Progesterone Receptor Testing in Breast Cancer: ASCO/CAP Guideline Update (2020)
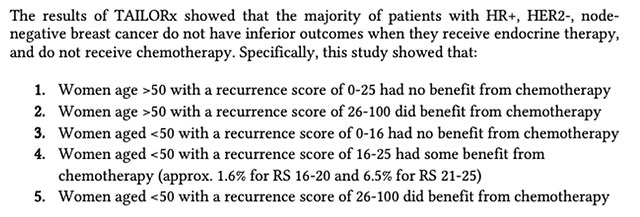
- Use of Biomarkers to Guide Decisions on Adjuvant Systemic Therapy for Women With Early-Stage Invasive Breast Cancer: ASCO Clinical Practice Guideline Update—Integration of Results From TAILORx (2019)
- Role of Patient and Disease Factors in Adjuvant Systemic Therapy Decision Making for Early-Stage, Operable Breast Cancer: Update of the ASCO Endorsement of the Cancer Care Ontario Guideline (2019)
- Fertility Preservation in Patients With Cancer: ASCO Clinical Practice Guideline Update (2018)
- Integrative Therapies During and After Breast Cancer Treatment: ASCO Endorsement of the SIO Clinical Practice Guideline (2018)
Neoadjuvant Chemotherapy, Endocrine Therapy and Targeted Therapy for Breast Cancer ASCO 2021
Management of Hereditary Breast Cancer in BRCA1/2 ASCO 2020
The American Society of Breast Surgeons (ASBrS)
- Consensus Guideline on Axillary Management for Patients With In-Situ and Invasive Breast Cancer: A Concise Overview (2022)
- Consensus Guideline on Genetic Testing for Hereditary Breast Cancer (2019)
- A Surgeon’s Resource Guide to Systemic Therapy in the Management of Hormone Receptor Positive Breast Cancer (2019)
- Position Statement on Screening Mammography (2019)
- Consensus Guideline on Breast Cancer Lumpectomy Margins (2018)
- Consensus Guideline on Venous Thromboembolism (VTE) Prophylaxis for Patients Undergoing Breast Operations (2018)
- Consensus Guideline on Diagnostic and Screening Magnetic Resonance Imaging of the Breast (2017)
- Performance and Practice Guidelines for the Use of Neoadjuvant Systemic Therapy in the Management of Breast Cancer (2017)
Systemic Therapy in the Management of Hormone Receptor Positive Breast Cancer- Oncotype DX ASBrS 2019
National Comprehensive Cancer Network (NCCN)
- Breast Cancer
- Genetic/Familial High-Risk Assessment: Breast, Ovarian, and Pancreatic
- Breast Cancer Risk Reduction
National Cancer Institute (NCI)
- Breast Cancer Treatment (2022)
- Breast Cancer Screening (2022)
- Male Breast Cancer Treatment (2021)
- Breast Cancer Prevention (2021)
- Breast Cancer Treatment During Pregnancy (2019)
The Society of Surgical Oncology (SSO)
- Society of Surgical Oncology–American Society for Radiation Oncology–American Society of Clinical Oncology Consensus Guideline on Margins for Breast-Conserving Surgery with Whole-Breast Irradiation in Ductal Carcinoma In Situ (2016)
- Society of Surgical Oncology–American Society for Radiation Oncology Consensus Guideline on Margins for Breast-Conserving Surgery With Whole-Breast Irradiation in Stages I and II Invasive Breast Cancer (2014)
American Society for Radiation Oncology (ASTRO)
- Radiation therapy for the whole breast: Executive summary of an American Society for Radiation Oncology (ASTRO) evidence-based guideline (2018)
- Postmastectomy Radiotherapy: An American Society of Clinical Oncology, American Society for Radiation Oncology, and Society of Surgical Oncology Focused Guideline Update (2016)
American Cancer Society (ACS)
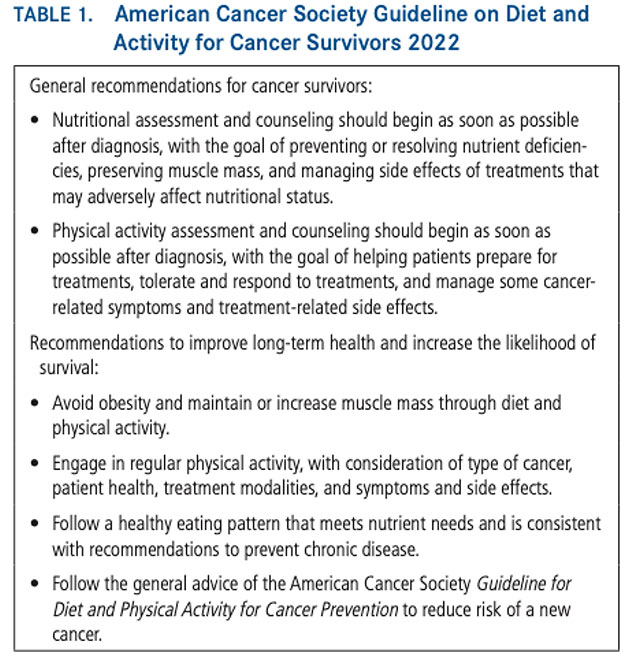
- American Cancer Society nutrition and physical activity guideline for cancer survivors (2022)
- American Cancer Society/American Society of Clinical Oncology Breast Cancer Survivorship Care Guideline (2016)
Guideline on Diet and Activity for Cancer Survivors ACS 2022
United Kingdom
National Institute for Health and Care Excellence (NICE)
- Familial breast cancer: classification, care and managing breast cancer and related risks in people with a family history of breast cancer (2019)
- Early and locally advanced breast cancer: diagnosis and management (2018)
- Tumour profiling tests to guide adjuvant chemotherapy decisions in early breast cancer (2018)
National Health Service (NHS)
ABS/BAPRAS
- Oncoplastic breast surgery: A guide to good practice (2021)
- Prepectoral implant-based breast reconstruction: a joint consensus guide from UK, European and USA breast and plastic reconstructive surgeons (2019)
Royal College of Radiologists (RCR)
Europe
European Society for Medical Oncology (ESMO)
- ESO-ESMO 4th International Consensus Guidelines for Breast Cancer in Young Women (2020)
- Systemic anticancer therapy-induced peripheral and central neurotoxicity: ESMO-EONS-EANO Clinical Practice Guidelines for diagnosis, prevention,
treatment and follow-up (2020)
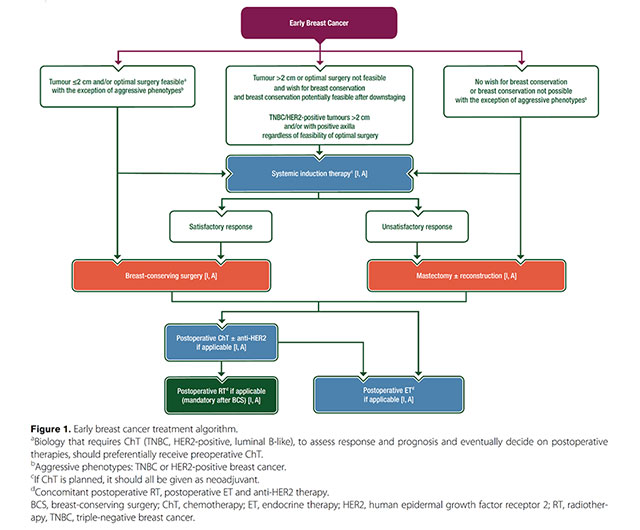
- Early breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up (2019)
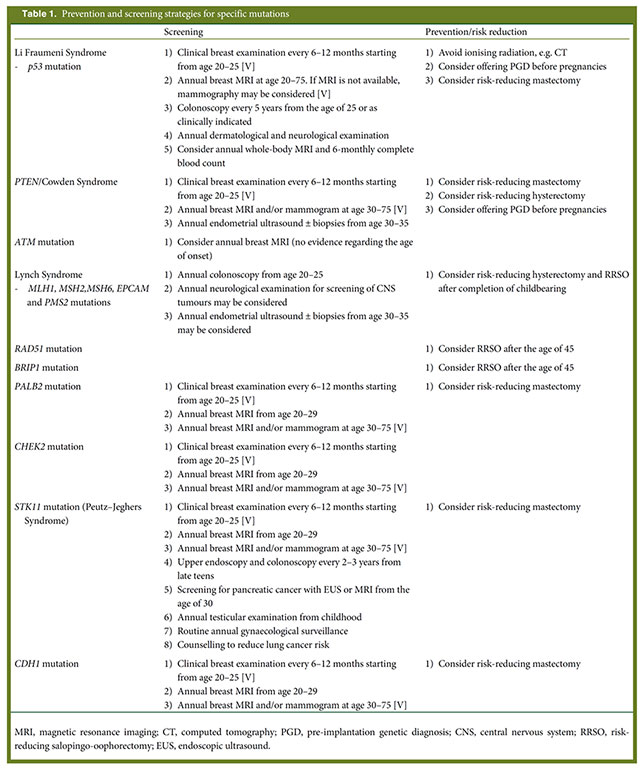
- Prevention and screening in BRCA mutation carriers and other breast/ovarian hereditary cancer syndromes: ESMO Clinical Practice Guidelines for cancer prevention and screening (2016)
Early Breast Cancer Treatment Algorithm ESMO 2019
Prevention and Screening Strategies for Specific Mutations ESMO 2016
European Society of Breast Cancer Specialists (EUSOMA)
- Updated recommendations regarding the management of older patients with breast cancer: a joint paper from the European Society of Breast Cancer Specialists (EUSOMA) and the International Society of Geriatric Oncology (SIOG) (2021)
- The requirements of a specialist breast centre (2020)
St Gallen
- Customizing local and systemic therapies for women with early breast cancer: the St. Gallen International Consensus Guidelines for treatment of early breast cancer (2021)
- St. Gallen/Vienna 2021: A Brief Summary of the Consensus Discussion on Customizing Therapies for Women with Early Breast Cancer (2021)
- Highlights of the 17th St Gallen International Breast Cancer Conference 2021: customising local and systemic therapies (2021)
- Estimating the benefits of therapy for early-stage breast cancer: the St. Gallen International Consensus Guidelines for the primary therapy of early breast cancer 2019
- St. Gallen/Vienna 2019: A Brief Summary of the Consensus Discussion on the Optimal Primary Breast Cancer Treatment 2019
- Highlights of the 16th St Gallen International Breast Cancer Conference,
Vienna, Austria, 20–23 March 2019: personalised treatments for patients with early breast cancer 2019 - De-escalating and escalating treatments for early-stage breast cancer: the St. Gallen International Expert Consensus Conference on the Primary Therapy of Early Breast Cancer 2017
- St. Gallen/Vienna 2017: A Brief Summary of the Consensus Discussion about Escalation and De-Escalation of Primary Breast Cancer Treatment 2017
- Highlights from the 15th St Gallen International Breast Cancer Conference 15–18 March, 2017, Vienna: tailored treatments for patients with early breast cancer 2017
- Tailoring therapies—improving the management of early breast cancer: St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2015
- 14th St. Gallen International Breast Cancer Conference 2015: Evidence, Controversies, Consensus – Primary Therapy of Early Breast Cancer: Opinions Expressed by German Experts 2015
- Highlights from the 14th St Gallen International Breast Cancer Conference 2015 in Vienna: Dealing with classification, prognostication, and prediction refinement to personalize the treatment of patients with early breast cancer 2015
European Society of Breast Imaging (EUSOBI)
Australia
Cancer Australia
- Guidance for the management of early breast cancer: Recommendations and practice points (2020)
- Recommendations for the management of early breast cancer in women with an identified BRCA1 or BRCA2 gene mutation or at high risk of a gene mutation (2014)
Clinical Oncology Society of Australia (COSA)
- Medications to lower the risk of breast cancer (2020)
- COSA Position Statement on Exercise in Cancer Care (2018)
Guidelines for Patients
NCCN
- Breast Cancer – Invasive (2022)
- Breast Cancer – Ductal Carcinoma in Situ (2022)
- Breast Cancer – Metastatic (2022)
NCI
- Breast Cancer Treatment -Patient Version (2022)
- Male Breast Cancer Treatment –Patient Version (2022)
- Breast Cancer Treatment During Pregnancy – Patient Version (2022)
- Breast Cancer Prevention–Patient Version (2021)
ABS/BAPRAS
ACS
ESMO
COSA
Breast Cancer Care Pathways
Cancer Australia/Cancer Council