Adjuvant Therapy
Your breast surgeon says the surgery to remove your breast cancer was a success, but then refers you on to other doctors, usually a medical oncologist and a radiation oncologist, to consider more treatment — called “adjuvant” therapy.
Why?
It has long been recognized that breast cancer is not always cured by locoregional treatment alone. To reduce the risk of distant and local recurrence, patients are usually offered “adjuvant” treatment. The aim of adjuvant “systemic” therapy is thought to principally be elimination of clinically undetectable micrometastatic disease and to reduce the chance of “distant” (metastatic) recurrence and the main aim of “local” therapy with radiation is to reduce “local” recurrence.
What is adjuvant therapy?
Adjuvant therapy is a term used to encompass all of the extra treatments given in addition to surgery to help reduce the chance of breast cancer recurrence.
“Adjuvant” therapy is used after the primary treatment, which is usually surgery, to lessen the chance of your breast cancer coming back. Even though your surgery was successful at removing all visible cancer, microscopic cancer cells that are undetectable with current methods may remain.

Adjuvant therapy for breast cancer is designed to treat “micrometastatic” disease, or breast cancer cells that have escaped the breast and regional lymph nodes, but have not yet established an identifiable metastasis.
By contrast, ‘neoadjuvant’ breast cancer therapy is given prior to any other treatments in order to improve the benefit of subsequent treatments.
Which treatments are used as adjuvant therapies?
Surgery only removes the cancer from the area it is in the body, and radiotherapy only treats the area of the body it is aimed at.
Doctors use drug therapies because they circulates throughout the body in the bloodstream, and so can treat cancer almost anywhere in the body. Drug therapies are “systemic” treatment.

Types of cancer treatments that are used as adjuvant therapy include:
- Chemotherapy uses drugs to kill cancer cells throughout the body.
- Hormone therapy.For cancers sensitive to hormones, certain treatments can stop hormone production in your body or block the effect of hormones. Hormonal therapy may be taken for 5-10 years.

- Targeted therapy.Targeted therapy is designed to alter specific abnormalities present within cancer cells. For example, targeted therapies are available to block the action of a protein called human epidermal growth factor receptor 2 (HER2) in women with breast cancer.

- Immunotherapy works with your body’s immune system to fight off any remaining cancer cells by stimulating your body’s own defenses or supplementing them. Immunotherapy is a relatively new approach in breast cancer treatment as a means of ‘amplifying’ the effectiveness of the body’s own defense systems.
- Radiation therapy.Radiation therapy uses high-powered energy beams to kill cancer cells. Radiation therapy may last 3 to 6 weeks.

How effective is adjuvant therapy?
Because none of these treatments is completely harmless, it’s important to determine the risks of adjuvant therapy versus the benefits. The following factors can help you and your doctor determine whether adjuvant therapy is appropriate for you and, if so, which type:
- Type of cancer.
- Stage of cancer.The stage refers to the extent of the cancer. If the cancer is at a very early stage — before it has had time to spread — then the chance of cancer recurring after surgery may be very small. Adjuvant therapy may offer little benefit in this case. But if a cancer has spread to nearby lymph nodes, adjuvant therapy may be more beneficial.
- Number of lymph nodes involved.
- Hormone receptivity.Hormone therapy won’t be effective if your cancer is not hormonally sensitive.
- Other cancer-specific changes.Certain cancers may have specific changes within their cells that indicate the likelihood that your cancer will return, making adjuvant therapy more likely to be beneficial. If tests show your cancer is unlikely to recur, adjuvant therapy may offer little benefit.
See:
Receiving adjuvant therapy doesn’t guarantee your cancer won’t recur. It can, however, help reduce the risk that your cancer will come back.
Is adjuvant therapy for you?
So, how do you decide whether adjuvant therapy is right for you? You might want to discuss the following issues with your doctor:-
- Which treatments may be effective for your case?
- What are the side effects?
- What are the changes you’ll stay cancer-free?
- How is your overall health?
- What is your preference?
Together you and your doctors can weigh these factors and decide whether the benefits of adjuvant therapy outweigh the risks for you.
The main aim of adjuvant “systemic “therapy is thought to be the eradication of micrometastatic disease which otherwise is the cause of relapse in the future. Studies have shown that cancer cells can lie dormant for many years despite radical treatment and cause recurrent disease. The difficulty is “proving” who has residual disease when there is no way clinically of detecting it. Understandably, this can be a difficult concept for patients to understand. Currently there is no gold standard algorithm or molecular test to determine the need or not of adjuvant treatment, but the chance of relapse is estimated using the prognostic features, individualized to each of the patients. Inevitably by this selection process, some patients will receive chemotherapy inappropriately, gaining no survival benefit, but potentially suffering acute and chronic side effects from the treatment. Even if we could prove that an individual patient did have micro-metastatic disease, could we then prove the treatment will work? Some patients will have chemorefractory or chemoresistant disease, and go through months of unnecessary treatment.
What is chemotherapy?
Chemotherapy is the use of drugs (medicines) to kill cancer cells. Chemotherapy medicines are also called ‘cytotoxic’ or ‘anticancer’ drugs. The aim of these medicines is to destroy any cancer cells in the body that may have escaped away from the breast into the bloodstream and other parts of the body. These cells are usually much too small to show up on X-rays or blood tests.

“Adjuvant” chemotherapy is chemotherapy that is used after surgery removes a cancer from the breast. Chemotherapy may also be “neo-adjuvant”; this is chemotherapy that is used to shrink a breast cancer before surgery.
How does chemotherapy work?
Chemotherapy stops cells from growing. Fast growing cells, like cancer cells, are most likely to be affected by chemotherapy drugs. Normal cells can be affected too, and that is why some people experience side effects with treatment. Normal cells recover from chemotherapy treatment but cancer cells don’t recover as effectively.

The breast cancer cure rate is at an all-time high, and so is the information, to say nothing of the misinformation, available to patients and their families. Online searches can lead to unreliable sources, leaving even the most resilient patient feeling uneasy and uncertain about her diagnosis, treatment options, doctors, side effects, and recovery. Adding to a patient’s anxiety is input from well-meaning friends and family, with stories, worries, and opinions to share, sometimes without knowing the details of her particular case, when in reality breast cancer treatment has gone well beyond a “one size fits all” approach.

As we have figured out the different types of breast cancer, we have become better able to match the treatments to the individual patient, both in terms of their risk of recurrence and the potential benefit of the therapy.
This is important, because none of the systemic therapies are without side effects, some of which can be quite significant. If a drug has prolonged your life, you might well put up with secondary heart problems or surgery for uterine cancer. If, however, you really did not need or benefit from chemotherapy, then developing leukemia as a result would be tragic. Although we are better nowadays at matching the treatment with the patient, there is still a grey zone.

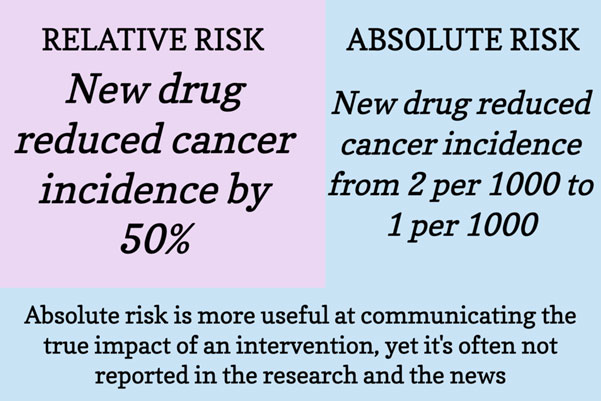
How much risk of recurrence is enough to justify a treatment? Physicians frequently use the threshold of greater than 90 percent disease-free survival at ten years with local therapy alone to define the women whose prognosis is too good to justify aggressive systemic therapy. Depending on your age, general health, and outlook on life, this might be what you would choose as well. However, it is worth taking the time to think about what you are willing to undergo for a statistical improvement in your odds. It is, after all, a bit of a gamble. For example if we consider that chemotherapy reduces the risk of recurrence by about a third, that means that the higher the chance of recurrence, the more beneficial the chemotherapy is likely to be for you. If you have a 60 percent chance of recurrence, a one-third risk reduction means chemo will reduce that chance by 20 percent, but if you have a 9 percent chance of recurrence, the one-third reduction is only 3 percent, although the effects are not perfectly linear. The absolute risk reduction of an intervention in your particular case is a much more important metric than the relative risk reduction of the intervention.
We tend to equate recurrence with death because at this time we are not usually able to cure a woman whose breast cancer comes back outside of the breast or axillary lymph nodes. As our drugs improve, however, this is starting to change, with many women living a long time with metastatic disease.
Although it is important to ask about statistics to get a sense of the seriousness of your situation, it is also important to remember that whatever happens to you is 100 percent! If 99 percent of women live and you die, you are still dead. And if 99 percent die and you live, you are still alive. This is an important concept to understand when trying to weigh risks and benefits.

It is always better to look at the absolute benefit of chemotherapy. In other words, if your chances of dying by ten years were 50 percent and you had a treatment that reduced the risk of mortality by 50 percent, your absolute benefit at ten years would be 25 percent. Another way to say this for those of you who find percentages difficult to follow, is if there were one hundred women with the same cancer as you, then fifty of them would be dead at ten years, having died within that time frame. If a treatment reduced the chance of dying by 50 percent, then twenty-five of them would be dead at ten years. And we have to remember that there are other things that can kill us, from car accidents to coronavirus.

Not all oncologists agree with this way of looking at the figures, and there is sometimes a bit of wishful thinking in their approach to chemotherapy. They want it to work, so they hope that it works better than it does. Thus, you need to pin your oncologist down so that you are realistic about the benefits of chemotherapy in your case.
Systemic therapy does not guarantee that your cancer will be cured; it may simply prolong the time to recurrence. But that in itself can be a worthwhile goal. The key, however, is actually to understand what the treatments are buying and weigh whether they are worth it.
Even considering the different types of breast cancer, it is impossible to tell what is going to happen with any one woman. All our prognostications are, of necessity, based on large statistical groups of patients, the long-term survival rates of the different kinds of breast cancer. You can see that if the triple-negative women get through the first five years, they do very well, while the women with oestrogen-positive tumours can have recurrences after five years! These prognostications have some use—as long as you realize they don’t absolutely predict the course of your particular disease. It is good to know how serious the situation could be, but whatever happens to you is 100 percent! If 99 percent of women with tumours like yours die and you survive, you have beaten the odds. On the flip side, the majority of women can be cured, and if your cancer comes back, you are in the unlucky small percentage. I think it is important to look at the statistics and get a sense of how serious the situation is so you can take care of what you need to, but then you should forget them because whatever happens to you is what is important, not the statistics!
Beware the medical oncologist who just talks about “relapse” or “recurrence,” which is also misleading because it over-inflates the chance of your cancer coming back. Relapse statistics include all sorts of “events” that cannot be controlled by chemotherapy, such as getting breast cancer on the other side (which is not reduced by chemotherapy), dying in a car accident or from another cause, and getting a cancer totally unrelated to breast cancer.
Understand what your baseline cure rate is without chemotherapy or hormonal treatment
- Understand what your chances of dying of other causes or old age are —if, for example, your chance of dying from other causes is high or much higher than dying from breast cancer
- Be careful of the oncologist who quotes odds ratios or odds reductions or reductions in the risk of relapse, as they may be making chemotherapy sound better than it is and may lead you into a decision that’s not absolutely necessary
- For patients who are older with hormone-positive tumours, hormone tablets such as tamoxifen and aromatase inhibitors may provide most of the benefit
- For younger women who are hormone sensitive, chemotherapy alone is not enough, and some sort of hormonal manipulation will also be necessary.
So the trick is not to be over-treated or under-treated.
Be careful of the oncologist who quotes only “relapse” statistics, as they may be making the benefit from chemotherapy sound better than it really is.
First, understand what your baseline survival rate is without chemotherapy or hormonal treatment. Also understand what your chances of dying of other causes or old age are to put your risk from breast cancer into perspective.
Statistics are only a guide to your prognosis at the point of diagnosis. Your chances improve over time, particularly after you reach five years post-diagnosis.
This additional or “adjuvant” treatment is, in some ways, a bit of extra insurance. Scientific evidence has shown that there is a greater chance of killing off cancer cells when they are small and invisible to the naked eye, before they become dangerous spots or breast cancer.
![]() Adjuvant Therapy Breast Cancer
Adjuvant Therapy Breast Cancer
![]() American Cancer Society-Treating Breast Cancer
American Cancer Society-Treating Breast Cancer
For more information on adjuvant therapies see Breast Cancer Patient Information Resources.
You will need the Adobe Reader to view and print these documents.
![]()











