Nipple – Sparing Mastectomy/Nipple Delay
Nipple-Sparing Mastectomy (NSM) is a type of mastectomy (see Types of Mastectomy ) in which the breast tissue is removed, but surgeons preserve the entire breast skin “envelope” including the nipple areola complex (NAC), which includes the nipple itself and the darker pigmented circle of skin that surrounds it (areola). Typically, breast reconstruction is performed immediately.
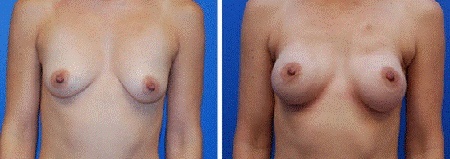
Above: Before and After Bilateral NSM and reconstruction via inframammary fold incisions
Despite a growing body of evidence showing that, with proper patient selection and operative technique, NSM is a safe and effective intervention for patients requiring therapeutic or prophylactic mastectomy, this type of surgery is not yet widely available, especially in Australia.
Nipple-sparing mastectomy is increasingly being considered as an alternative to skin-sparing mastectomy (in which the nipple areolar complex is sacrificed) in both the therapeutic and prophylactic settings, as patient satisfaction and a positive impact on body image have been demonstrated repeatedly. For women with BRCA mutations who choose mastectomy, preservation of the NAC may be even more important due to the generally younger age at time of surgery.
Despite the potential for improved cosmetic and psychological benefit, nipple-sparing mastectomy is still not widely offered, because of the dual concerns for oncologic safety and surgical risk of these more ambitious surgical techniques. In the United States, reports from multiple centres have confirmed that prophylactic and therapeutic nipple-sparing mastectomies can be consistently performed with low recurrence and complication rates and NSM is slowly entering the mainstream for both the treatment and prevention of breast cancer.
NSM was in the past known as “subcutaneous mastectomy”. In the 1970’s, subcutaneous mastectomy was occasionally performed for fibrocystic disease, breast cancer prevention and less frequently for cancer. By the 1980’s, reports of cancer occurring in the residual breast tissue led the procedure into disfavour. It was not until the last few years that this procedure regained popularity. Removal of the NAC at time of mastectomy has been based on longstanding concerns by surgeons about possible tumour recurrence or the development of a new primary tumour in the remaining tissue, as well as the postoperative viability of the NAC relating to it’s blood supply.
The major concerns with nipple-sparing mastectomy can be categorized as oncologic and surgical. The oncologic concerns for the procedure are (1) the risk of cancer occurring anywhere in the breast or beneath the nipple-areola complex, either de novo or recurrent (for those patients who had cancer), and (2) the difficulty in performing an adequate mastectomy through the limited incision for the nipple-sparing mastectomy, possibly leading to an inadequate therapeutic procedure. The surgical concern for the procedure is the possibility of increased perioperative wound complications, such as ischemic necrosis of either the nipple-areola complex or the longer and larger mastectomy skin flaps.
The oncologic safety of nipple-sparing mastectomy should be considered within the spectrum of lumpectomy, skin-sparing mastectomy, and modified radical mastectomy. Well-controlled trials have clearly demonstrated the oncologic equivalence of modified radical and skin sparing mastectomies with the risk of future breast cancer recurrence low, but not zero. Comparing skin-sparing mastectomy with lumpectomy, the incidence of cancer recurrence is higher in patients with lumpectomy, but a crucial finding from 20- and 25-year follow-up studies is that there is no statistically significant difference between mastectomy and lumpectomy in terms of disease-free survival, distant disease-free survival, and overall survival.
Multiple retrospective studies from different institutions have repeatedly found a low long-term incidence of cancer development in the nipple-areola complex following nipple-sparing mastectomy for therapeutic and prophylactic indications. Several single-institution groups have reported their outcomes with wide variations in local recurrence rates and with median follow-up intervals often shorter than 2 years. In contrast, reports of larger sample sizes with longer follow-up have also demonstrated low local recurrence rates. For example, a 21-year study published in the November 2011 issue of the journal Plastic and Reconstructive Surgery, of 162 nipple-sparing mastectomies conducted between 1989 and 2010 found no new cancers or cancer recurrences among the patients. Author Scott Spear, professor of plastic surgery at the Georgetown University Hospital, where the study took place, cautions that the “nipple-sparing technique is not appropriate for every patient depending upon their anatomy and type of breast pathology. Careful selection of the right patient for NSM is an important element of success.”
The accumulating data from multiple series of NSM certainly show that carefully selected patients have a low risk of local cancer recurrence, that recurrences occur rarely in the nipple, and that recurrences in the nipple can be managed by removing the nipple. The goal of nipple-sparing mastectomy is to produce outstanding cosmetic results with little or no sacrifice of oncologic or surgical safety. For this concept to be worthwhile to the patient, there must be agreement that the goal of improved cosmesis is achieved, and is worth the possible increased oncologic risk even if it is believed to be small.
Recognizing which patients are at risk for pathologic NAC involvement is ideally done preoperatively for both surgical planning and patient education. A variety of factors have previously been reported as being associated with nipple involvement in patients with breast cancer, including larger tumor size, shorter tumor-to-nipple distance, central location, lymphovascular invasion, lymph node metastases, advanced stage and grade, younger age and extensive in situ component. A study recently published in Ann Surg Oncol (Billar et al, 2011) however demonstrated that clinical and imaging abnormalities at the NAC were the only independent preoperative predictors of NAC pathology, and the absence of these factors conveys a low probability of NAC involvement.
The modern term “nipple-sparing mastectomy” now refers to a more radical surgical removal of breast tissue than was carried out during the subcutaneous mastectomy era. To minimize residual ductal elements at the NAC base and to reduce the risk of leaving occult tumour, the dissection and removal of tissue should be carefully and thoroughly performed using an “inverted sock” technique, as pictured below.
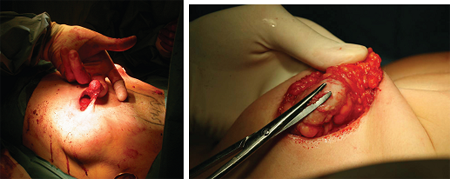
Most protocols for nipple-sparing mastectomy involve analysis of subareolar tissue as a separate biopsy and the final decision to spare the nipple must ultimately await frozen and then definitive pathologic section. With the exception of invasive cancer at the margins, resection of the nipple for positive margins can be delayed until the second stage of the reconstructive surgery.
In Jane O’Brien’s surgical practice, all patients who undergo nipple-sparing mastectomy for malignancy either undergo retroareoalar biopsy at the time of pre mastectomy sentinel node biopsy/nipple delay or intraoperative frozen-section pathological analysis of the tissue shavings behind the nipple. If positive for tumour, the nipple is removed.
In the case of intraoperative frozen section, care is taken to thoroughly counsel patients preoperatively to ensure they are aware of this potential outcome. Furthermore, if a patient is scheduled for bilateral NSM, it is clarified in advance how the contralateral nipple should be addressed in the event that one nipple requires removal.
Who is a suitable candidate for NSM?
There are two main issues governing the selection of candidates for nipple-sparing mastectomy:
- Oncologic safety -will this safely treat the cancer without leaving any behind?
- Cosmesis -will this enhance the appearance of the reconstructed breast?
Patients who have large cancers that are close to the nipple run the risk of leaving residual cancer cells in the nipple. These patients are not good candidates for this procedure. The surgeon may often predict if this is a risk before surgery with modern, sophisticated imaging studies such as MRI.
Nipple preservation may not be cosmetically ideal in patients who have large, pendulous breasts (C/D-cup or greater). In these patients, the cosmetic effect of nipple preservation may be less than optimal and until now, the option of a nipple-sparing mastectomy has been largely limited to women with relatively small and minimally sagging or ptotic breasts. Even this is changing, with the possibility of extending the indications, so that now some breasts that were previously felt to be too large or ptotic, can be considered for nipple sparing mastectomy, by employing a staged procedure. The first stage involves reducing the breast size or degree of ptosis by performing a mastopexy (lift) or reduction followed at least three or four weeks later by the second stage -nipple-sparing mastectomy and reconstruction. This approach is particularly suited to the risk reduction setting where the time delay between the two stages is not problematic. In the breast cancer setting, the staged approach must be carefully planned, so that it does not significantly delay or hinder cancer treatment. One option is to perform the mastopexy or reduction at the time of the tumour lumpectomy, before chemotherapy, and nipple-sparing mastectomy and reconstruction can then be performed on completion of chemotherapy.
The goal of the breast cancer surgeon is to optimize the patient’s cosmesis and quality of life while minimizing breast cancer risk. To achieve this goal, NSM should only be performed in carefully selected patients. To optimize cosmesis, candidates should be those who will likely have minimal reconstructive complications, such as women who are not obese and who are nonsmokers, Patients with pendulous/ptotic breasts are often poor candidates because of the location of the native NAC in the reconstructed breast and the inability to achieve symmetry.
There are a variety of incisions that have been used for NSM. The most popular include the inferolateral inframammary crease, lateral radial, the circumareolar with lateral extension, the vertical lower breast and the “omega” incision which can be used in conjunction with mastopexy/skin envelope reduction.
The inframammary crease approach offers a chance to place the skin scar away from the breast proper and hide it in a natural skin fold. This incision works best in patients with a small breast cup size, little ptosis, and a manageable distance between the incision site and the upper-inner extent of the glandular breast tissue.

Inframammary crease incision
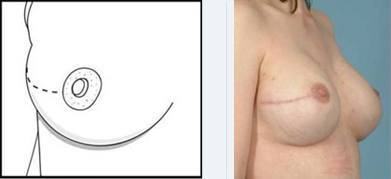
Lateral Radial Incision
Vertical Incision Circumareolar with lateral extension

Omega (mastopexy) Incision
With all of the described incisions, the skin flaps are typically longer and more vulnerable than conventional mastectomy flaps. Therefore, it is critical that dissection should be done expeditiously by a skilled surgeon. Flap-loss rates are directly related to counter traction time. It is venous congestion (more than arterial blockage) that leads to devastating flap loss. Flaps should therefore be raised as quickly as expertise will allow. For more difficult dissections it is prudent to periodically relax tension on the flaps.
NIPPLE DELAY
Surgical complications related to nipple-sparing surgery are not unusual. The ability to oxygenate the breast skin is related to the blood supply, and the blood supply to the nipple and areola particularly may be in jeopardy following NSM. Necrosis (tissue death), with either partial or total loss of the nipple-areola complex, has been noted in virtually all reported series of nipple-sparing mastectomy. It appears to vary from a high near 20% to a low of 2-3%, with most series reporting an incidence of around 10%. Many factors account for the differences, including choice of incision, breast size (increase risk in larger breasts) and on how radically the breast tissue from behind the nipple and areola is removed.
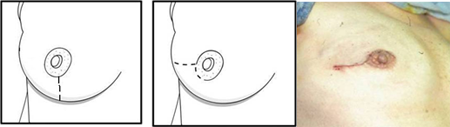
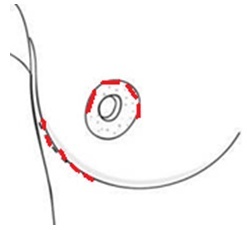
To reduce the chance of nipple necrosis, consideration may sometimes be given to performing a surgical “nipple delay” procedure. “Nipple delay” is intended to create new circulatory connections from the breast skin to the nipple/areolar complex, and involves dividing the blood vessels and other breast tissue beneath the nipple, so that the nipple is no longer dependent on the underlying breast tissue for it’s blood supply. Over the next 1 – 3 weeks, this remaining blood supply becomes much more robust and the blood flow to the nipple-areola from the surrounding skin increases. The nipple then becomes accustomed to receiving it’s blood supply from the skin around it, instead of the breast tissue underneath, which can potentially help it survive the subsequent nipple-sparing mastectomy procedure.
“Nipple Delay” procedures are performed a couple of weeks prior to nipple-sparing mastectomy, usually via the incision planned for the subsequent mastectomy, as pictured below.
REFERENCES:
![]() Surgical Delay of the Nipple–Areolar Complex
Surgical Delay of the Nipple–Areolar Complex
![]() Delay techniques for nipple-sparing mastectomy: A systematic review
Delay techniques for nipple-sparing mastectomy: A systematic review
![]() Protecting Nipple Perfusion by Devascularization and Surgical Delay
Protecting Nipple Perfusion by Devascularization and Surgical Delay
![]() Surgical delay may extend the indications for nipple-sparing mastectomy
Surgical delay may extend the indications for nipple-sparing mastectomy
![]() Staged Breast Operations: The Nipple Delay as an Old and New Idea
Staged Breast Operations: The Nipple Delay as an Old and New Idea
VIDEO
SUMMARY
Nipple sparing mastectomy (NSM) is one of the more notable surgical advances in breast cancer treatment and prevention. It is a surgical technique similar to the traditional mastectomy in that the whole breast is removed, but unique in that it spares the entire skin envelope including the nipple and areola and is accompanied by immediate reconstruction. While limited surgery and breast preservation is an appropriate surgical option for a large number of breast cancer patients, at least 25% of patients will still require, or desire, mastectomy, and by preserving the nipple, the psychological burden of mastectomy can be greatly reduced.
NSM is much more technically challenging than other forms of mastectomy and it is especially important therefore that you ensure your surgeon has considerable expertise in the technique. NSM is not very widely performed in Australia as yet, and you should consider specifically ask your surgeon how many NSM he/she has performed in the last year. If it is very few, or none at all, you may wish to seek a second opinion from a surgeon who performs the nipple sparing procedure frequently.
Jane O’Brien has a special interest in NSM, which she performs regularly. She feels the available evidence supports it’s oncological safety in very carefully selected patients and that the only absolute preoperative oncological contraindication (apart from locally advanced or inflammatory breast cancer or Paget’s disease of the nipple) is strong clinical or imaging suspicion of NAC tumour involvement. Consideration should be given to preoperative MRI to further exclude nipple involvement.
See Photo Gallery– Nipple Sparing Mastectomy for examples of NSM.











