Incisions/Scars for Benign Breast Lump Removal
IMPORTANT-PLEASE NOTE:
- NONE OF THE IMAGES ON THIS WEBSITE ARE OF ACTUAL PATIENTS OF JANE O’BRIEN
- THE IMAGES ARE PROVIDED FOR YOUR INFORMATION AS EXAMPLES ONLY
- ALL IMAGES IN THE PHOTO GALLERY HAVE BEEN SOURCED FROM THE PUBLIC DOMAIN
- JANE O’BRIEN FEELS THAT OUT OF RESPECT FOR HER PATENTS, PRE AND POST OP PHOTOS ARE MOST APPROPRIATELY SHARED IN AN OFFICE CONSULTATION AND NOT ON THE INTERNET. SHE IS HAPPY IF APPROPRIATE TO REVIEW RELEVANT DE-IDENTIFIED PRE AND POST OPERATIVE PHOTOS OF HER OWN PATIENTS IN THE PRIVACY OF HER OFFICE WHEN YOU MEET WITH HER
Incisions/Scars for Benign Breast Lump Removal
Jane O’Brien feels strongly that the final cosmetic appearance is important after all forms of breast surgery. This is particularly so after the removal of benign (innocent) breast lumps, as their removal on occasions may not be absolutely medically essential.
All surgery results in scars. Every time the skin is cut in surgery, a scar is produced. Everybody scars differently and some people scar more easily than others. The ideal end-result of any breast surgical procedure is a good quality scar which is well placed and able to be camouflaged. Scars take time to settle. The lumpiness, puckering and thickening in the scar takes at least 2-3 months to diminish, whilst the redness and pigmentation can take up to 9-12 months to fade. Most scars become flat and pale after 12 months. The width of the scar is dependent on the amount of scar ‘stretch’. Cross-hatching of the scar (horizontal lines across the length of the scar like the rungs of a ladder as shown in the photo below) can be avoided by using buried, dissolvable stitches.

Factors affecting scar formation
The quality and appearance of scars vary widely with the following factors:
- The individual’s healing process
- The position of the scar on the breast
- The degree of tension placed on the scar
Every individual forms different types of scars. These are determined by:
- Personal factors
- Nutritional State. Protein and vitamin deficiency can impede collagen synthesis and thus wound healing
- Underlying medical conditions e.g. diabetes, vascular disease
- Some medications (e.g. steroid therapy) may limit the healing process
- The age of the patient can also be a factor. Generally, younger skin makes thicker scars because it so vigorously heals itself. Getting older often means less visible scarring.
- Bleeding tendencies or vascular diseases can affect wound healing
- Lifestyle. Smoking, sun exposure and not following post-operative instructions all contribute to more visible scarring. Smoking decreases the body’s ability to transport oxygen through the bloodstream. This means that your body has less oxygen to help it heal after surgery. Scars will not only heal more slowly, they may not fade to their maximum potential. Sun exposure will tan scars, making them more visible.
- Genetic traits in scar formation
- Racial and ethnic background
Many of the above factors are beyond the control of the surgeon, and often cannot be predicted before surgery. As surgeons, we try to hide scars in natural lines, and to camouflage their existence if possible. We also employ particular suturing techniques to maximise the quality of the scar.
Unfavourable scars
Every surgery carries the risk of developing unfavourable scars. These are scars which have characteristics that make it difficult to be camouflaged, such as lumpiness, thickness and significant discolouration.
Some factors which may predispose to unfavourable scarring are:
- Wound infections
- Wound dehiscence (where the wound opens up 2-3 weeks after surgery)
Some patients can form hard, red, thick hypertrophic scars which cannot be anticipated by the surgeon before the operation. The type of scarring produced by any previous surgeries may give an indication to the type of scarring that might result. In the worst cases, these scars will take one to two years to reduce in thickness and will never end up as thin line scars. Scars will nearly always mature and flatten, but the time interval for this to occur is variable, from several months to several years
Ways to optimise your scars
It is important to follow the post-operative instructions given to you by your surgeon. These are given to minimise the chances of infection, decrease wound breakdown, and unfavourable scarring. Miss O’Brien recommends that the steristrips and supportive transparent dressing remain on the wound for approximately 14 days post op. The wounds are at their weakest at 2-3 weeks (when the wound has only 60-70% normal skin strength and the sutures have started to dissolve – thus losing their strength). This is the period when the wound is most vulnerable to dehiscence (breaking apart). It is important that no excessive force or tension is applied to the edges of the wound.
The colour of your scar
Surgical scars, when settled or mature, are white (they contain no pigment producing cells) but occasionally scars can over pigment (i.e. become darker). This is usually due to sun exposure but can be exacerbated in certain skin types, oral contraceptive pill (and other hormone treatment) and certain drugs. To minimise the colour change, it is always important to protect the scar from sun exposure in its early stages. Sunscreen use is essential.
Incisions
For breast cancer surgery the placement of the incision will be dictated to a degree by the cancer. In contrast, in the removal of benign (innocent) breast lumps it should usually be possible for incision placement to take into account the cosmetic result. It is almost always possible to avoid making an unfavourably placed incision if careful consideration is given preoperatively to the options. Scars in potentially visible locations (eg cleavage) should be avoided. Both cases below show less than ideal scar placement.




Favourable Incisions
The circumareolar or periareolar incision is made in the semi-circle around the outline of the areola, or the brown/ pink pigmented region surrounding the nipple The incision is placed so the scar blends in with the darker skin of the areola. The scar from a periareolar incision may be virtually invisible, as it blends well with the natural change in skin color. The inframammary incision is made in the crease/fold underneath the breast.
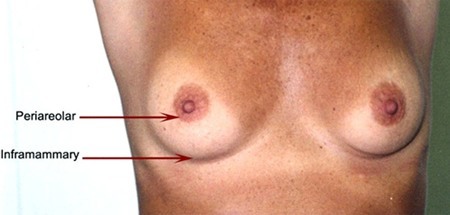


Almost all benign lumps can potentially be removed via either a circumareolar or inframammary incision. It may take the surgeon longer, be a little more uncomfortable postoperatively for the patient and be technically more difficult for the surgeon, however in Jane O’Brien’s opinion the resultant scar is superior and makes the additional effort worthwhile. Quite large benign lumps such as fibroadenomas can be removed via fairly small periareolar incisions as shown below.

Below are examples of periareolar and inframammary scars.
Periareolar/Circumareolar Scars














Inframammary Scars















