Ductal Carcinoma in Situ (DCIS)
TBC Ductal Carcinoma In Situ (DCIS)
What is DCIS?
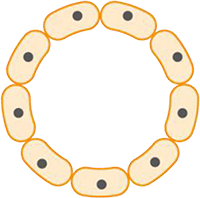
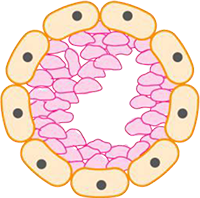
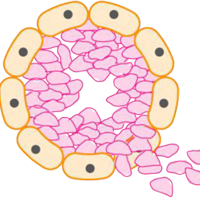
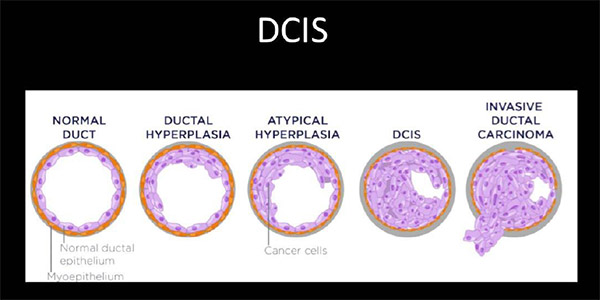
Ductal carcinoma in situ (DCIS) means the cells that line the milk ducts of the breast have become cancer, but they have not spread into surrounding breast tissue. Ductal Carcinoma in Situ (DCIS) is an early form of breast cancer and accounts for about 20% of all breast cancers. DCIS is diagnosed more often now than in the past. It is often picked up in women when they have mammograms as part of the Australian breast screening programme.
DCIS is considered non-invasive or pre-invasive breast cancer. DCIS can’t spread outside the breast, but it still needs to be treated because it can sometimes go on to become invasive breast cancer (which can spread).
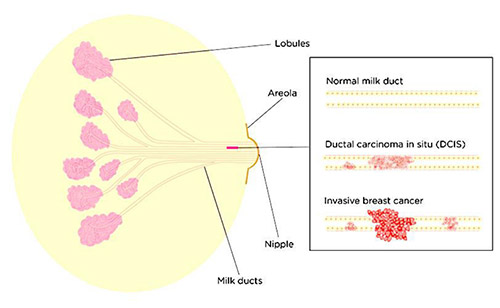
Breast cancer starts when cells in the breast begin to divide and grow in an abnormal way. Breasts are made up of lobules (milk-producing glands) and ducts (tubes that carry milk to the nipple), which are surrounded by glandular, fibrous and fatty tissue. When cancer cells have developed within the ducts of the breast but remain within the ducts (‘in situ’), it is called DCIS. The cancer cells have not yet developed the ability to spread outside these ducts into the surrounding breast tissue or to other parts of the body. As a result of being confined to the ducts, DCIS has a very good prognosis.
Is DCIS a type of cancer?
This is a controversial topic, partly due to the language. It has the word “carcinoma” in the name, and it is classified as stage 0 cancer. So DCIS isn’t life-threatening, but it has the potential to become invasive cancer.
You may hear DCIS described in different ways such as a pre-invasive, intraductal, non-invasive cancer.
What’s the difference between DCIS and invasive breast cancer?
The abnormal cells seen in DCIS are cancer cells. However, DCIS is not breast cancer as we commonly understand it. In breast cancer, the cancer cells have spread out of the milk ducts into the surrounding breast tissue. That is why it’s sometimes called ‘invasive’ breast cancer.
What are the symptoms of DCIS?
DCIS usually has no symptoms. Most cases of DCIS are found during routine breast screening or if a mammogram (breast x-ray) is done for some other reason.
Before commencement of screening mammography in Australia, DCIS made up only 2% of all newly diagnosed breast cancers. It usually presented with a palpable mass or was associated with another abnormality such as nipple discharge or Paget disease of the nipple, with or without a mass. It now represents around 20% of all newly diagnosed breast cancers detected by BreastScreen, Australia’s national screening program.
DCIS is still occasionally found when people have a breast change such as a lump or discharge from the nipple. However, if someone with DCIS has a breast change it’s more likely they will also have an invasive breast cancer. Some people with DCIS also have a type of rash involving the nipple known as Paget’s disease of the breast, although this is rare.
How is DCIS diagnosed?
If you have no symptoms and are recalled following a mammogram it may be because some tiny white dots were seen on the mammogram. These white dots are called calcifications. Calcifications can be due to DCIS. However, not all calcifications are found to be DCIS. Many women develop benign calcifications in their breasts as they get older.
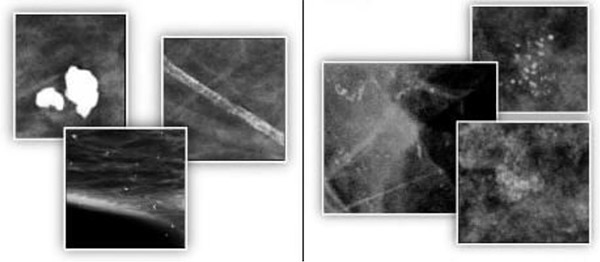
Calcifications are small calcium deposits in the breast that show up as white spots on a mammogram. Large, round or well-defined calcifications (shown above left) are more likely to be noncancerous (benign). Tight clusters of tiny, irregularly shaped calcifications (shown above right) may indicate DCIS.
If you have calcifications, further mammograms will be done to see the calcifications in more detail. Sometimes an ultrasound will also be done.
If the calcifications are not clearly benign, you’ll have an image-guided biopsy to help make a diagnosis. This is where samples of breast tissue are taken using a mammogram to help locate the exact position of the calcifications. Sometimes an ultrasound is used but this is less common. The biopsy samples will be x-rayed to check if they contain calcifications before being sent to the laboratory to be examined under a microscope.
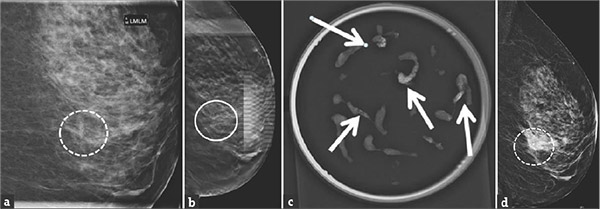
A 55-year-old woman called back after routine mammographic screening for calcifications in the left breast.
(a) Magnification view shows new grouped fine pleomorphic calcifications in the lower inner quadrant of the left breast (dashed circle). (
- b) Tomosynthesis images clearly demonstrate the calcifications (circle).
(c) Specimen radiograph shows the calcifications (arrows).
(d) Post biopsy mammogram demonstrates the marker clip in the targeted area.
Pathology result showed ductal carcinoma in situ.
If you have a biopsy, sometimes a small metal clip (or marker) is placed in the breast where the biopsy samples were taken. This is so the area can be found again if another biopsy or surgery is needed. It can safely be left in the breast and does not need to be removed, even if no further procedures are needed.
There are various histological patterns of DCIS and more than one of these may be present in a single case. The most common are the comedo, solid, papillary, cribriform and micro-papillary types. The biological potential for a subsequent invasive carcinoma may differ among the types of DCIS. Cells of the comedo type are cytologically more malignant, more likely to be high grade than other types of DCIS and have a higher proliferative rate.
Although in the majority of cases the diagnosis of DCIS is straightforward, DCIS may be difficult to differentiate histologically from (benign) atypical ductal hyperplasia (ADH) at one end of the spectrum, and invasive carcinoma at the other. Myoepithelial stains are used to help identify a breach in the duct lining.
How is DCIS graded?
DCIS is graded based on what the cells look like under the microscope. DCIS is graded as low, intermediate, or high grade.
- low grade – the cancer cells look most like normal cells and are usually slow-growing
- intermediate grade – the cancer cells look less like normal cells and are growing faster
- high grade – the cancer cells look most changed and are usually fast-growing
Natural history of DCIS
Ductal carcinoma in situ is considered a precursor of invasive breast cancer. There is a 30–50% risk of untreated DCIS progressing to invasive carcinoma in the ipsilateral breast 10–20 years after initial diagnosis. The cumulative risk of contralateral breast cancer is low (less than 1% per annum).
When there is occult invasion or lymph vessel or node involvement, the tumour is considered to be an invasive carcinoma. Occult invasion may be present in up to 20% of cases; up to 50% when the tumour is 50 mm or more.
In some cases, DCIS will never develop further or grows so slowly that it would never cause harm during that person’s lifetime. Although the size and grade of the DCIS can help predict if it will become invasive, there is currently no way of knowing if this will happen. High-grade DCIS is more likely to become an invasive breast cancer than low-grade DCIS and do so more quickly.
Can DCIS be left untreated?
Because there’s no way of knowing when or if DCIS will become invasive, treatment is usually recommended. It is possible that this may lead to unnecessary or overtreatment for some people.
The aim of treatment is to remove all the DCIS from within the breast to reduce the chance of it becoming an invasive cancer.
Research is ongoing to identify which cases of DCIS will go on to become invasive and which might be safe to leave untreated. If you are diagnosed with low-grade DCIS, you may be invited to join a clinical trial.
Why is DCIS treated?
The aim of treating DCIS is to prevent invasive breast cancer from developing. If DCIS is not treated it may develop into invasive breast cancer, which can spread outside the ducts into the breast tissue and then possibly to other parts of the body.
We don’t know for certain how many women with DCIS would develop invasive breast cancer if they were not treated. Also, it is not possible to predict which women with DCIS will develop invasive breast cancer if they were not treated or how long after the diagnosis of DCIS an invasive breast cancer would develop. Some women with DCIS may never develop any problems if they are not treated. However, some women with DCIS may develop invasive breast cancer.

Because DCIS may develop into invasive breast cancer and invasive breast cancer can spread and cause death, women with DCIS are generally recommended to have treatment. Treatment for DCIS aims to help prevent invasive breast cancer from developing and DCIS from coming back in the breast.
DCIS can be treated successfully and most women diagnosed and treated for DCIS will not later develop invasive breast cancer.
A focus of current research effort is to identify whether treatment for DCIS can vary dependent on the grade of the disease. There are currently international clinical trials, the LORIS, LORD and COMET trials, in the UK, Europe and the USA respectively that are investigating the “watch and wait” approach compared to immediate treatment for the management of low-grade DCIS. The results from these trials will help to determine the best treatment options for women with low-grade DCIS. At this time, however, there are no national or international guidelines which recommend a “watch and wait” management option for low-grade DCIS.
How is DCIS treated?
Surgery
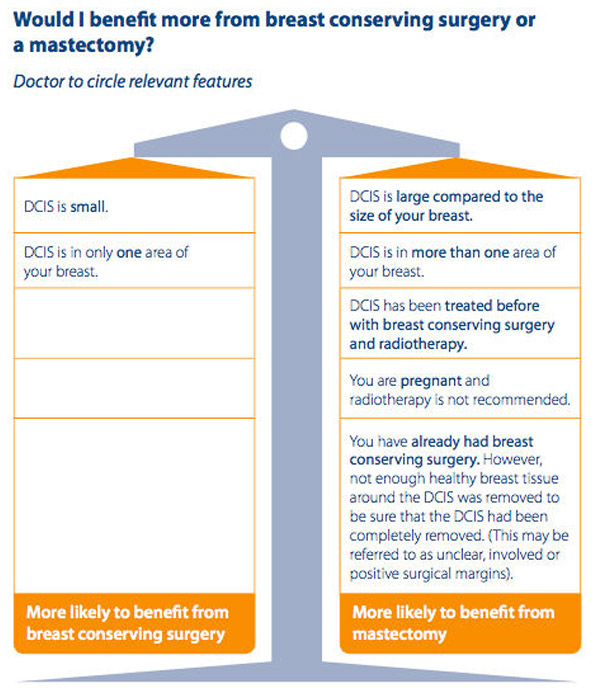
Surgery is nearly always the first treatment for DCIS. This may be breast-conserving surgery (also known as a wide local excision or lumpectomy) or mastectomy. A nipple-sparing mastectomy may be possible in some cases.
You may be offered a choice between these types of surgery, depending on the size and location of the area affected. Your breast surgeon will discuss this with you.
While DCIS is usually detected as an area of microcalcification, it is known that not all DCIS will calcify. The size of a cluster of microcalcification on mammography may therefore underestimate the true extent of the lesion. Breast MRI may be useful in providing additional information regarding the local extent of DCIS within the breast.

A mastectomy is more likely to be recommended if:
- You have a large area of DCIS. If the area is large relative to the size of your breast, a lumpectomy may not produce acceptable cosmetic results.
- There are more than one area of DCIS or the DCIS is in more than one part of the breast (multifocal or multicentric disease). It’s difficult to remove multiple areas of DCIS with a lumpectomy. This is especially true if DCIS is found in different sections — or quadrants — of the breast.
- It hasn’t been possible to get a clear margin of normal tissue around the DCIS with wide local excision
- You’re not a candidate for radiation therapy. Radiation is usually given after a lumpectomy.
- You may not be a candidate if you’re diagnosed in the first trimester of pregnancy, you’ve received prior radiation to your chest or breast, or you have a condition that makes you more sensitive to the side effects of radiation therapy, such as systemic lupus erythematosus.
- You prefer to have a mastectomy rather than a lumpectomy.

Patient
- Breast size (small breast in relation to tumour size)
- Preference (mastectomy, or to avoid radiation therapy)
- Risk factors (including age and family history)
- Relative or absolute contraindications to radiation therapy (eg. connective tissue or genetic disorders)
- Pregnancy (use of radiotherapy to be avoided until after delivery)
Tumour
- Large area of DCIS
- Diffuse malignant appearing microcalcifications throughout entire breast
- Multifocal tumours or multicentric tumours (involving different quadrants)
Treatment factors
- Positive margins following wide local excision and re-excision neither possible
nor suitable - Residual calcifications on mammogram
- Recurrent tumour after previous breast conservation
- Radiation therapy inaccessible
- Previous ipsilateral breast irradiation
If you have breast-conserving surgery, the breast tissue removed during surgery is examined by a pathologist. If any cancer cells are seen at or close to the margin, you may need more surgery to get a clear margin.
If a mastectomy is not recommended but you would prefer to have one, you can discuss this with your surgeon.
As most cases of DCIS can’t be felt, a procedure called localisation is often used on the day of breast-conserving surgery. This helps mark the exact area to be removed during surgery. Using a mammogram (breast x-ray) or an ultrasound as a guide, a very fine wire is inserted into the area of concern. When a mammogram is used, your breast is compressed throughout the procedure. You’ll be given a local anaesthetic to numb the area but you may still feel some discomfort. Once the wire is inserted, a mammogram is taken to check that it is in the correct position. Once the wire is in the correct place, it’s secured with a padded dressing and left there until surgery when it’s removed.
Some hospitals are using a new localisation procedure where instead of a fine wire, a tiny very low dose radioactive seed (about the size of a grain of rice) is inserted into the breast tissue. This can be done up to two weeks before your operation. At surgery a special probe is used to locate the seed and guide the surgeon to the tissue that needs to be removed along with the seed.
If you’re having a mastectomy you’ll usually be able to have breast reconstruction. This can be done at the same time as your mastectomy (immediate reconstruction) or months or years later (delayed reconstruction). Some women choose not to or cannot have a breast reconstruction. They may use a breast prosthesis or may prefer not to use anything.
Lymph node removal
Most people with DCIS won’t have surgery to remove the lymph nodes. People with invasive breast cancers will usually have lymph node removal, to check if any of the lymph nodes under the arm contain cancer cells. This helps decide whether or not any additional treatment will be of benefit.
Sometimes an area of invasive breast cancer is found as well as DCIS. If so, it will affect the treatment(s) you’re offered and you may need surgery to the lymph nodes from under the arm to check if they contain cancer cells.
Lymph node removal is not usually recommended for people with DCIS alone undergoing lumpectomy because the cancer cells haven’t developed the ability to spread outside the ducts into the surrounding breast tissue and cannot therefore have spread to the lymph nodes.
However, if you’re having a mastectomy your specialist will discuss having a sentinel lymph node biopsy at the same time as it can be more difficult to assess the lymph nodes later if any invasive breast cancer is found in the mastectomy specimen.
Sometimes an area of invasive breast cancer is found as well as DCIS. If so, it will affect the treatment(s) you’re offered and you may need surgery to the lymph nodes from under the arm to check if they contain cancer cells.
Is surgery always necessary for DCIS?
We nearly always recommend surgery. Even though DCIS is non-invasive and not life-threatening, it has the potential to turn into something more serious. Furthermore, when we do surgery for DCIS, 20% of the time we find an invasive cancer in the tissue that we did not know about from the needle biopsy. For this reason, the only time we don’t do surgery for DCIS is when we think the risks of the surgery don’t outweigh the benefits. For example, some patients might not be able to tolerate the procedure because of their age or other health problems.

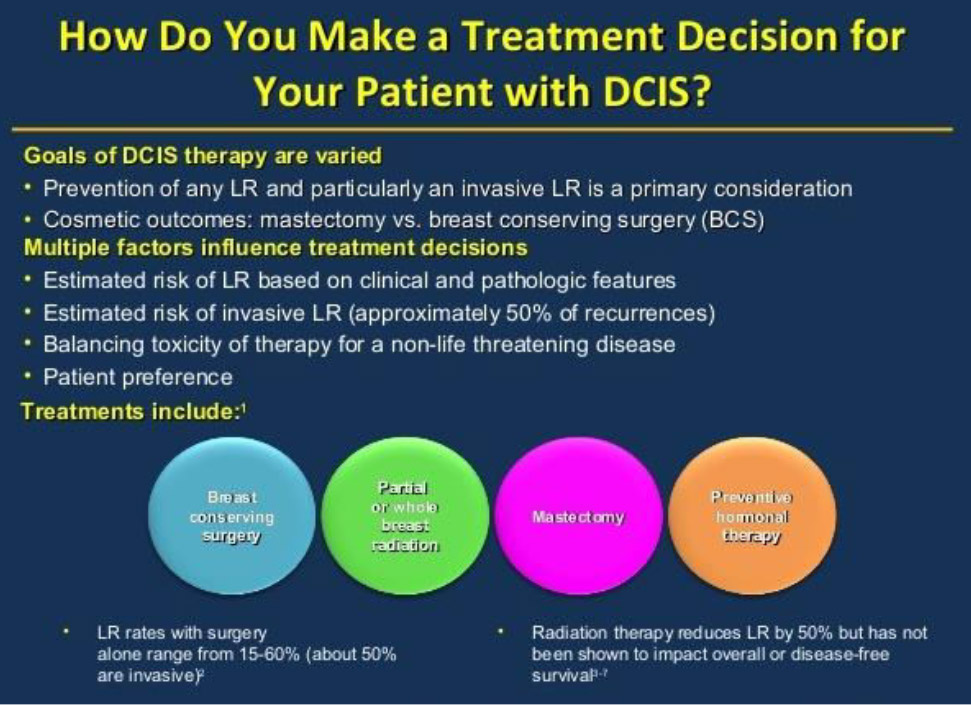
Are any additional (adjuvant) treatments required?
After surgery, you may need other treatments. These are called adjuvant treatments and can include radiotherapy and, in some cases, hormone therapy. The aim of these treatments is to reduce the risk of DCIS coming back or an invasive cancer developing.
Chemotherapy and targeted (biological) therapy are not used as treatment for DCIS.
For women who have a mastectomy for DCIS, there is usually no need for additional treatment, because the risk of the cancer coming back is very low.
The main argument for a mastectomy is that it is curative in nearly all patients, but may represent overtreatment for many women. In a large review, 1.6% of the 1565 patients treated with mastectomy developed a local recurrence, of which 72% were invasive. Survival was excellent at 98–100%. A meta-analysis elicited a similar local failure rate of 1.4% for studies involving mastectomy alone.
Radiotherapy
Radiotherapy uses high energy x-rays to destroy cancer cells. If you’ve had breast-conserving surgery you may be offered radiotherapy. It is unnecessary to have radiotherapy after a mastectomy for DCIS.
Often the hardest decision faced by women with DCIS is whether to have radiotherapy after a lumpectomy. A lot of factors must be considered, including the size and grade of the DCIS, how close the DCIS cells were to the final margin, and the age of the person at diagnosis. Younger women have a higher risk of recurrence. And then as a surgeon, I need to consider how each of my patients thinks about risk. For example, a 10% risk of recurrence in the next ten years can mean completely different things to two different people. Some women want to do everything to lower their risk, while others are happy to just have it watched closely.

Local recurrence rates are reduced by at least 50% when RT is added to BCS. This was demonstrated in three large randomised controlled trials (RCT) published in the late 1990s and early 2000s comparing BCS with or without RT, and was confirmed in a meta-analysis. The meta-analysis demonstrated a statistically significant reduction in local recurrences from 22.5% with studies employing BCS only, to 8.9% for BCS and RT. The most apparent differences were for those patients with high grade tumours, DCIS with necrosis, tumours of the ‘comedo’ subtype, or DCIS with close or positive surgical margins.
LR=local recurrence
The NSABP B-17 trial reported a reduction in the frequency of ipsilateral breast tumours from 31% at 8 years to 13% with the addition of postoperative irradiation. Mortality was 1.6% for the entire cohort. Despite only a 4 year follow up, the other two RCTs, also showed a statistically significant reduction in local recurrence. These and other studies reiterate that close to 50% of the local recurrences were invasive carcinoma and the other 50% were carcinoma in situ.
The dilemma for the radiation oncologist is the uncertainty about who may safely be treated with surgery alone, avoiding RT. There may be some patients with very small or low grade tumours for whom RT will not sufficiently alter their prognosis.
Hormone (endocrine) therapy
All invasive breast cancers are tested for hormone receptors (oestrogen and progesterone) receptors. DCIS may be tested for these hormone receptors , but it is not routinely undertaken in some countries.
The evidence for the use of endocrine therapy in the treatment of DCIS is unclear, and the results of the two large RCTs comparing BCS and RT with or without tamoxifen are conflicting. Tamoxifen therapy is not routinely recommended, but it may be considered for selected patients.
Tamoxifen therapy is therefore not routinely recommended, but it may be considered for selected patients.
How likely is DCIS to come back?
The chance of the DCIS coming back depends on various factors. But after mastectomy DCIS almost never comes back. In women who have just the area of DCIS removed the chance of it coming back is a bit higher. But it depends on the grade and type of DCIS.
Ductal carcinoma in situ may recur after treatment. Factors increasing the risk of local recurrence after breast conservation include:
- young age at diagnosis
- increasing tumour size
- positive margins
- high grade tumours, and
- the omission of radiotherapy.
After treatment for DCIS, half the recurrences following surgery with or without radiation are invasive carcinoma, while half are DCIS.

Mastectomy represents the most radical treatment, and obviates the need for follow up imaging of the ipsilateral breast required after breast conserving techniques. It is often difficult for patients with DCIS (a noninvasive condition) to accept recommendation for mastectomy for a condition that is not invasive when paradoxically, BCS and XRT is frequently offered to treat invasive carcinoma.
Local recurrence rates following conservative surgery alone without XRT is in the order of 22.5%. In one study, approximately one-half of the recurrences were invasive cancer and one-half were DCIS. The short term survival rates were 98–100%, but as there is a greater risk of local recurrence with time, the longer term survival rates are likely to be lower. Patients undergoing breast conserving surgery alone need to be informed that their risk of a subsequent invasive cancer may be as high as 10%.
What is the optimal treatment for a local recurrence?
Although local recurrences are uncommon after initial treatment for DCIS, they can be psychologically devastating for the patient, particularly if it is an invasive recurrence. The treatment of a recurrence depends on the initial treatment of DCIS, whether the recurrence is DCIS or invasive, and whether the patient has received radiotherapy to the breast. After diagnosis is confirmed histologically, a screen for distant metastatic disease is usually performed.
For a patient treated by BCS alone, management options may include re-excision followed by radiation (XRT) or mastectomy with or without breast reconstruction. If BCS and XRT were used initially, then mastectomy is usually the only option available. If mastectomy alone was the original treatment modality, then surgical removal of a chest wall recurrence may be possible, followed by chest wall RT, but this situation is extremely rare. Treatment of the axilla and consideration of systemic therapy is also required. Most recurrences can be salvaged by mastectomy. One study showed that following mastectomy, subsequent freedom from chest wall recurrence was high (92% at 5 years).
Conclusion
Patients diagnosed with DCIS usually have an excellent outcome, with low local recurrence rates and a survival of at least 98%.

The diagnosis of DCIS may be distressing for the patient, particularly if it is a screen detected lesion in a well woman without breast symptoms. The patient can be reassured that it is not invasive disease but a form of ‘pre- cancer’, that long term survival is high, and that in most patients DCIS does not recur. Patients should be given all options objectively. Some women prefer the added ‘security’ of having a mastectomy but for many women this represents overtreatment. Conservative surgery is an acceptable form of treatment that is associated with low rates of recurrence, low rates of salvage mastectomy, and low rates of invasive recurrence, and is the preferred treatment for many women.
DCIS: PATIENT INFORMATION
TBC Ductal Carninoma In Situ DCIS
Understanding DCIS MACMILLAN Cancer Support 2023
NBOCC DCIS Understanding Your Diagnosis And Treatment
Breast Cancer Action DCIS Factsheet