Breast Reconstruction and Post-Mastectomy Radiotherapy (PMRT)
![]() Breast Reconstruction and Post Mastectomy Radiotherapy (PMRT)
Breast Reconstruction and Post Mastectomy Radiotherapy (PMRT)
Choosing the Most Appropriate Form of Breast Reconstruction when Post-Mastectomy Radiation (PMRT) is Required
 There is currently no clear consensus on the optimal management and timing of breast reconstruction in the setting of recommended or possible post mastectomy radiation therapy (PMRT). Radiation can have deleterious effects on the cosmetic outcome of reconstructive procedures, and as a result, the timing of reconstruction in women who may require PMRT is a heavily debated topic.
There is currently no clear consensus on the optimal management and timing of breast reconstruction in the setting of recommended or possible post mastectomy radiation therapy (PMRT). Radiation can have deleterious effects on the cosmetic outcome of reconstructive procedures, and as a result, the timing of reconstruction in women who may require PMRT is a heavily debated topic.
Some surgeons consider PMRT to be a relative contraindication to immediate reconstruction, and advise women to undergo mastectomy, PMRT, and then reconstruction 6 to 12 months later. Other surgeons take into consideration the psychological and technical benefits of immediate reconstruction and recommend it, recognizing that outcomes in these women may on occasions be suboptimal, although still equivalent or superior to delayed reconstruction.
Historically, most plastic surgeons have not recommended autologous tissue flap reconstruction in patients who will require PMRT. Instead, these patients have either undergone “delayed” reconstruction or “delayed-immediate” reconstruction, with insertion of a tissue-expander or an implant as a temporising procedure, with a view to delayed autologous reconstruction being undertaken after radiation.
What was resulting with this practice in my experience, was that a significant proportion of these patients, “battle weary’ after their breast cancer treatment, and not keen on further major surgery, did not proceed with autologous reconstruction, instead “making do” with an irradiated implant based reconstruction, which was quite frequently cosmetically suboptimal, and often also uncomfortable.
Emerging evidence now shows that immediate autologous breast reconstruction can tolerate radiotherapy better than previously thought. The American Mastectomy Reconstruction Outcomes Consortium (MROC), a five-year prospective study, was designed to compare the outcomes of the two major categories of breast reconstruction: autologous and implant-based. It is the largest study to date to evaluate the impact of PMRT on breast reconstruction results, and showed higher rates of complication and failure in radiated women who had implant reconstruction compared with autologous breast reconstruction. Patients who had implants were more than 2 ½ times more likely to experience complications than those with autologous reconstruction, and within the first two years, 11% of radiated patients with implants experienced reconstructive failure, compared with 3% of non-radiated patients. Researchers concluded that “radiation therapy compromises the outcomes of implant reconstruction but NOT of autologous reconstruction”.
The presentation of the MROC study data at the annual San Antonio Breast Cancer Symposium (SABCS) in December 2016, which has since been published in the Journal of the National Cancer Institute (JNCI) (1) was the turning point for me. I felt with the existing local protocol, in which plastic surgeons were recommending against immediate autologous reconstruction in patients requiring PMRT, that I was, based on the most up to date scientific evidence, potentially denying my patients their best reconstructive option. As such, I made a firm decision to change how I was practicing. I now counsel patients that immediate autologous reconstruction is a good option in those who require PMRT, which has led to a significant change in my reconstructive practice with a dramatic increase in immediate autologous reconstruction, and a complete reversal in the ratio of autologous (tissue flap) vs alloplastic (implant based) reconstruction.
CHANGES IN SURGICAL PRACTICE:
The last 2 years (2017/2018) has seen a very significant change in my practice in the type of immediate breast reconstruction performed at the time of mastectomy for cancer in comparison to previous years, with a reversal in the ratio of autologous (tissue flap) vs alloplastic (implant based) reconstruction.
In 2018, 82% of all immediate reconstructions performed at the time of mastectomy for malignancy were autologous, and in 2017 57%, compared to 26% in 2016 and 21% in 2015.
Between Oct 2017 and Dec 2018, all 24 of my patients requiring PMRT and undergoing immediate reconstruction, have ALL undergone immediate autologous flap reconstruction.
| Immediate Reconstruction at the time of Mastectomy for Malignancy (prophylactic, risk-reduction mastectomies with immediate reconstruction excluded) |
2015 | 2016 | 2017 | 2018 |
| Autologous Recon (% of overall immediate recon) |
21 | 26 | 57 | 82 |
| Implant Based Recon (% of overall immediate recon) |
79 | 74 | 43 | 18 |

Many women undergoing mastectomy hope to avoid radiation therapy because of a range of potential harms, including skin changes and fibrosis. Although many patients who have a mastectomy can avoid radiation, therapy there are patients, including those with nodal disease (4 or more involved nodes and and increasingly, 1-3 involved nodes), for whom PMRT is recommended/considered in order to reduce the risk of local recurrence. Because of the tissue damage from radiation, these women may have more problems with reconstruction surgeries. There are a range of different kinds of reconstruction, which can be separated into two broad categories; implant based and autologous reconstruction. Not all patients are not necessarily candidates for autologous reconstruction, which is a long and involved procedure.
In patients who pursue implant reconstruction, potential complications related to radiotherapy include scarring, capsular contracture, infection, pain, skin necrosis, fibrosis, and impaired wound healing. Patients who pursue autologous reconstruction may also face radiotherapy-related complications, including fat necrosis, fibrosis, atrophy, and flap contracture.

The MROC study included 662 radiated and 1,625 nonirradiated postmastectomy patients who received either implant or autologous reconstruction at 11 institutions in the United States between 2012 and 2015. The median age of patients was 49 years. The study endpoints included complication rate, failure rate, and patient-reported outcomes.
- 662 women had radiation
- 1625 women didn’t have radiation
About 38% of the women who had radiation had autologous reconstruction and 62% had implant reconstruction
- About 25% of the women who didn’t have radiation had autologous reconstruction and 75% had implant reconstruction
Although a higher proportion of women who received postmastectomy radiotherapy received autologous reconstruction (37.9%) than unirradiated women (25.0%), implant techniques were still the most common approach observed in this multicentre cohort, even in the setting of radiotherapy. Other studies have demonstrated a dramatic increase in the use of implant reconstruction over time. This trend may be partly driven by patient preferences to minimize the acute morbidity, operative time, hospitalization, and recovery time. Of course, not all patients are candidates for autologous techniques, and not all patients would potentially choose an autologous approach over implants, even if aware of the complication and outcomes data.

Overall, 1 year after radiation was completed:
- 8% of women who had radiation had at least one complication
- 3% of women who didn’t have radiation had at least one complication
Two years after radiation was complete:
- 1% of women who had radiation had at least one complication
- 5% of women who didn’t have radiation had at least one complication
Two years after radiation treatment was completed:
- About 39% of women who had radiation after implant reconstruction had at least one complication (22% in non irradiated)
- 26% of women who had radiation after autologous reconstruction had at least one complication (28% in non irradiated)

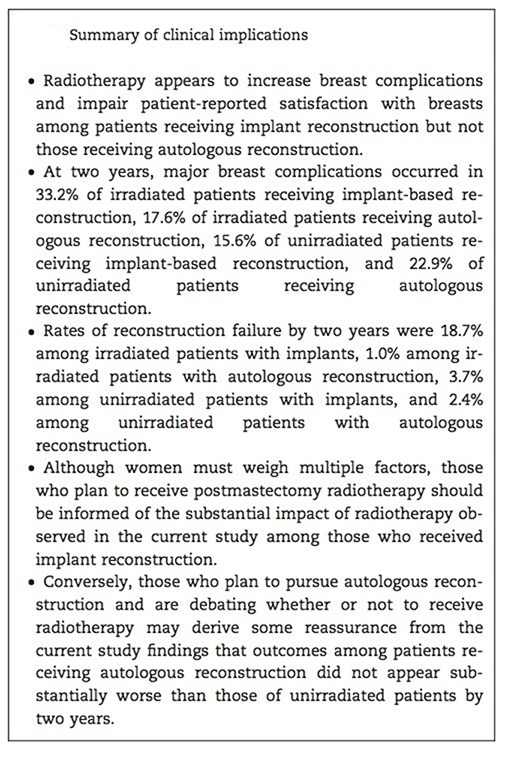
Overall, radiation was linked to more than doubling the risk of complications in women who had implant reconstruction, but was not associated with a higher risk of complications in women who had autologous reconstruction.
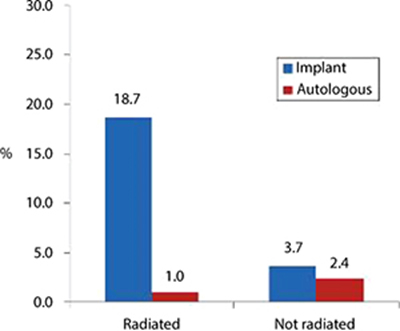
Reconstruction failure
By two years, reconstruction failure occurred in 11.4% of radiated patients and 3.4% of non-irradiated patients. Rates of reconstruction failure by two years were 18.7% among irradiated patients with implants, 1.0% among irradiated patients with autologous reconstruction, 3.7% among unirradiated patients with implants, and 2.4% among unirradiated patients with autologous reconstruction.
When the researchers looked at how the women rated their satisfaction with their reconstruction results, they found that among women with implant reconstruction, those who were treated with radiation were less satisfied than women who didn’t receive radiation. There were no differences in satisfaction among radiated and non-radiated women who received autologous reconstruction.
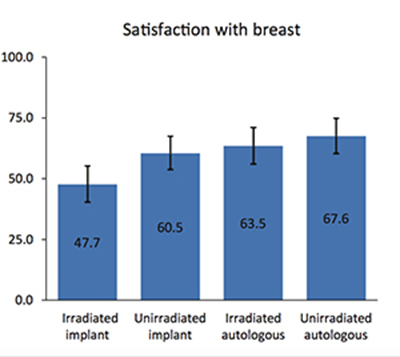
Patient-reported outcomes on the BREAST-Q (a validated quality-of-life instrument) were consistent with these findings. Radiated patients had a lower satisfaction rate with their reconstruction than nonirradiated patients and were more satisfied with outcomes of autologous breast reconstruction than implant reconstruction. A sub-study of MROC, discovered that women who elected for autologous reconstruction had greater overall satisfaction with their breasts than those who chose implants, and reported better outcomes on other quality of life measurements. The study, published in the Journal of Clinical Oncology-JCO (3), found that women who underwent autologous breast reconstruction, reported greater psychosocial and sexual well-being than those who chose implant-based reconstruction.
CONCLUSION:
Radiation therapy compromises the outcomes of implant reconstruction but NOT of autologous reconstruction. The main takeaway point from this large prospective trial is that radiation compromises the outcome of implant reconstruction. Autologous reconstruction appears to have superior patient-reported outcomes and a lower risk of complications than implant-based approaches in patients receiving radiation. Patients who had implants were more than 2 ½ times more likely to experience complications than those with autologous reconstruction, and within the first two years, 11% of radiated patients with implants experienced reconstructive failure, compared with 3% of non-radiated patients.

COMMENTARY:
Although women must still weigh multiple factors, including their suitability, differences in operative time and rehabilitation required for different approaches, when selecting their preferred type of reconstruction, those who are likely to receive post-mastectomy radiation therapy should be informed of the substantial and significant impact of radiotherapy observed among patients who received implant reconstruction. Conversely, those who wish to pursue autologous reconstruction may derive some reassurance from the current study findings that outcomes among patients receiving autologous reconstruction did not appear substantially worse than those of non-irradiated patients by two years.
The appreciation that radiation has a negative impact on implant-based reconstruction is not new. What is new, is finally some robust evidence that radiation does NOT have a markedly negative affect on autologous reconstruction. Many plastic surgeons have been (and many still continue to remain) reluctant to offer autologous flap reconstruction to patients who require or are anticipated to require post mastectomy radiotherapy, leaving the patient with the often less acceptable options of implant based reconstruction followed by radiotherapy, “delayed-immediate” reconstruction, in which a two-stage approach comprising a tissue-expander or implant in the first stage, and subsequent autologous reconstruction or delayed reconstruction. This new research adds strong support to the contention that immediate flap reconstruction is an appropriate option to offer suitable women who require or are strongly anticipated to require radiotherapy, and has already had a major influence on my own personal breast cancer surgical practice, as evidenced by the very significant increase in the proportion of autologous flap reconstructions in 2017and 2018, compared to preceeding years.
TAKE HOME MESSAGES FOR PATIENTS:
- If you know you’re likely to require post mastectomy radiation, and if you are suitable for a flap reconstruction, autologous reconstruction is likely to better tolerate the effects of radiation than an implant based reconstruction.
- As plastic surgeons ultimately determine access to autologous microvascular breast reconstruction, a change in surgical practice of this nature cannot occur in isolation, and breast surgeons who are themselves persuaded by recent research, and who wish to offer their patients the option of immediate autologous reconstruction in the setting of PMRT need to work alongside a plastic surgeon who is also willing to embrace the current evidence.If your treatment team, and the plastic surgeon to whom your breast surgeon has referred you, does not offer the option of autologous reconstruction in suitable women who require, or are likely to require, post-mastectomy radiotherapy (PMRT), you may wish to consider seeking a second opinion. This will usually mean seeking the opinion of a whole new treatment team, and you will need to obtain a referral from your GP to another breast surgeon, who will then arrange for onward referral to a plastic surgeon in their team.
- If you are undergoing neoadjuvant chemotherapy prior to breast cancer surgery, and the planned surgery is to be a mastectomy, it is a good idea to meet with a plastic surgeon early on during your neoadjuvant chemotherapy, as this then allows adequate time for you to seek a second surgical opinion if desired. Surgery is ideally undertaken around 3-4 weeks following completion of neoadjuvant chemotherapy, and given the complexity and length of flap surgery, it is usually in this circumstance, (ie in women undergoing neoadjuvant therapy), scheduled many weeks in advance. If you leave it until you have completed chemotherapy to seek a second opinion, it may not be possible from a practical point of view to do so, as there may be insufficient time to see a second treatment team and if appropriate reschedule your surgery within the recommended 4 week window period.
For further information on radiation and breast reconstruction, see Breast Care Network Australia (BCNA) Beacon Magazine, October 2018.
1. BCNA Breast Reconstruction![]() Click here for more information
Click here for more information
2. Jagsi et al, Impact of Radiotherapy on Complications and Patient- Reported Outcomes After Breast Reconstruction, JNCI J Natl Cancer Inst (2018)![]() Click here for more information
Click here for more information
3. Solin, L. Interaction of Postmastectomy Radiation Treatment With Breast Reconstruction: Many Questions, Emerging Data, JNCI (2018)![]() Click here for more information
Click here for more information
4. Pusic et al, Patient-Reported Outcomes 1 Year After Immediate Breast Reconstruction: Results of the Mastectomy Reconstruction Outcomes Consortium Study, JCO (2017)![]() Click here for more information
Click here for more information
5. Discussion: Should Immediate Autologous Breast Reconstruction Be Considered in Women Who Require Postmastectomy Radiation Therapy? A Prospective Analysis of Outcomes, JCO (2017)![]() Click here for more information
Click here for more information
6. Article: Should Immediate Autologous Breast Reconstruction Be Considered in Women Who Require Postmastectomy Radiation Therapy? A Prospective Analysis of Outcomes, JCO (2017)![]() Click here for more information
Click here for more information
7. Radiotherapy in the setting of breast reconstruction: types, techniques, and timing, Lancet Oncology (2017)![]() Click here for more information
Click here for more information
You will need the Adobe Reader to view and print these documents.![]()











