Axillary Surgery including Sentinel Node Biopsy
Axillary Surgery Following Neoadjuvant Chemotherapy- Multidisciplinary Guidance (2019)
Management of the Malignant Axilla in Early Breast Cancer-ABS Consensus Statement (2015)
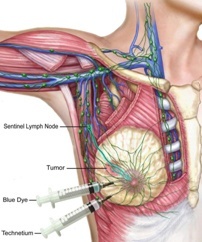
What is a sentinel lymph node?
The sentinel node/s are the lymph nodes that the breast drains to first, and are the first lymph nodes to which cancer cells are most likely to spread from a primary breast tumour. Usually, there is more than one sentinel lymph node.
What is Sentinel Lymph Node Biopsy (SLNB)?
A sentinel lymph node biopsy (SLNB) is a procedure in which the sentinel or ‘guardian’ lymph nodes are identified, removed, and pathologically examined to determine whether cancer cells are present. It is thought that if breast cancer cells were to escape into the lymphatic system, they would travel to the sentinel nodes before moving on to other nodes and the sentinel lymph node (SLN) technique is based upon the observation that tumour cells migrating from a primary tumour metastasise to one or a few lymph nodes before involving other lymph nodes.

SLNB is a minimally invasive and accurate alternative to axillary lymph node dissection (ALND) and is associated with reduced morbidity compared with axillary dissection. It aims to avoid some of the side effects of axillary dissection /clearance by removing fewer glands. During a sentinel lymph node biopsy, the surgeon removes only a few (usually approx one to five ) sentinel lymph nodes, whereas in an axillary node dissection commonly around twenty nodes or more are removed.
Removing only the sentinel or ‘guardian’ nodes lessens the likelihood of complications and in most cases still provides the necessary information about the cancer. If the sentinel nodes are free of cancer, it is assumed that the remaining nodes are also clear and no further lymph nodes are then removed.
There are still some situations when axillary clearance is needed, and if cancer cells are found in the sentinel node then axillary clearance is still often recommended. For women with clinically suspicious lymph glands or nodes that look abnormal on preoperative imaging, needle biopsy (often image guided) may provide a means to identify some patients who have positive involved nodes preoperatively, and who thus require axillary lymph node dissection rather than SLNB.
Sentinel node biopsy is a relatively new procedure, however most surgeons have adopted SLNB as a standard means of axillary nodal assessment. It is very important that sentinel node biopsy is done by a surgeon who is trained and experienced in this technique.
It has been shown that not only do increased overall volume of SLNB procedures lead to decreased failure rates, but also surgeons with high monthly averages of SLN biopsies have fewer failures than those with low monthly averages. (Cox et al, J Am Coll Surg, 2001) When viewed according to the surgical volume (cases per month) versus the success rate, three groups were identified. Surgeons performing fewer than three SLN biopsies per month had an average success rate of 86.23% (failure rate 13.77%), surgeons performing three to six SLN biopsies per month had a success rate of 88.73% (failure rate 11.27%) and surgeons performing more than six SLN biopsies per month had a success rate of 97.81% (failure rate 2.19%) again underlining the advantages of specialisation, and being treated by a high caseload breast surgeon. (See Benefits of Specialisation ) Ask your surgeon how many SLNB cases he/she performs per month.
What are Lymph Glands/Nodes?
The lymphatic system is a system of lymph vessels and lymph glands throughout the body which play an important role in the body’s mechanism of fighting infections and tumours. Tiny channels (called lymphatics) carry fluid and debris to the lymph nodes/glands which act as filters. Groups of lymph nodes are located in the neck, underarms, chest, abdomen, and groin. The lymph nodes that filter waste fluid and cells from the breast are mainly located in the armpit (also called the axilla.) These lymph nodes are usually the first ones affected if cancer spreads beyond the breast. The number of lymph nodes in the axilla varies from person to person but usually ranges from around 20 to 40.
Why is it important to know whether tumour cells are present in the glands under the arm?
The status of the axillary lymph nodes is one of the most important prognostic factors in women with early stage breast cancer, and because imaging techniques have limited sensitivity, the axilla must be explored surgically and some lymph nodes removed and submitted for pathological examination . Pathological examination of lymph nodes is the most accurate method for assessing spread of disease to these nodes to inform decisions about treatment and prognosis. Very important decisions regarding the overall treatment of breast cancer may be based on whether the lymph glands contain tumour cells.
The treatment of early breast cancer involves surgery to remove the breast tumour (lumpectomy or mastectomy) and also assessment and management of the axilla.
The approach to axillary assessment has traditionally been axillary dissection (or axillary clearance) in which a significant number of lymph nodes are surgically removed. This technique is associated with significant morbidity, particularly lymphoedema (permanent swelling of the arm due to a build-up of fluid in the tissues) Two prospective randomized trials and several prospective nonrandomized series have concluded that lymphoedema after SLNB is less common or severe than after ALND, however many of these studies do not report the actual incidence of lymphoedema. Of those that do, the reported rates of lymphoedema vary from 0% to 7% at 6 to 36 months after SLNB. Obesity, increasing BMI, and weight gain are commonly recognized as risk factors for lymphoedema and this appears to be the case for both SLNB and ALND. A study from the Memorial Sloan Kettering Cancer Centre documented lymphoedema rates at 5 years of 5% following SLNB and 16% following ALND. Higher body weight/BMI was a significant risk factor associated with the presence of lymphoedema at 5 years in both groups (JCO, 2008)
Only about 30% of women diagnosed with early breast cancer have positive axillary lymph nodes at diagnosis, and therefore two-thirds of patients will receive no benefit
from axillary dissection but are at risk of the morbidity associated with the procedure.
On the other hand however, it does appear that since the introduction of SLNB and as the number of published papers on the SLNB technique has increased, that the perceived complication rate of ALND has increased dramatically. Women who have involved nodes and require an ALND for oncological reasons can be reassured by the fact that with a 16% lymphoedema rate at 5 years, the vast majority of patients do not experience lymphoedema.
How are the sentinel lymph nodes identified?
Jane O’Brien uses the three methods described below to identify sentinel lymph nodes as the combination of all three techniques has been demonstrated to be the most accurate. These techniques produce a ‘road map’ to help the surgeon find the sentinel node for removal during the operation.
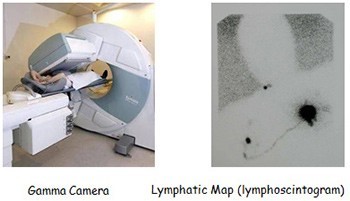
- Sentinel Node Imaging : Lymphatic mapping is performed the day before, or on the morning of surgery within the nuclear medicine department. A small amount of radioactive material is injected into the breast (injection of the radioactive isotope sometimes stings.) The radioactive tracer travels to the sentinel nodes, along the same lymphatic channels that cancer cells could travel and can be seen on a nuclear medicine scan (lymphoscintogram). Lymphoscintigraphy can also identify atypical drainage patterns to internal mammary, intramammary, interpectoral or infraclavicular nodes.This scan only shows where the sentinel node is located, but not whether it contains tumour or not.
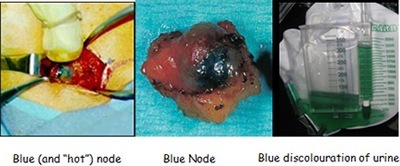
- Blue Dye Injection : The blue dye is injected into the breast once the patient is asleep in theatre. This dye travels to and stains the sentinel nodes blue, thereby assisting the surgeon to find the correct lymph nodes.

The blue dye discolouration may be visible following surgery on the nipple, but usually fades over the following weeks or months. Some of the blue dye passes into the bloodstream and is passed out in the urine, which may turn blue for 24 hours after surgery. There have been rare instances (less than 1 in 5000 cases- NBOCC 2009) of allergy to the dyes used in sentinel node biopsy. Allergic reactions are usually mild and easily treatable.
- Gamma probe detection : A hand-held gamma probe (a type of Geiger counter) used in the operating theatre guides the surgeon to the radioactive material injected preoperatively.
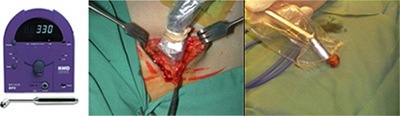
Gamma Probe”Hot” node identified Probe held to “hot” node
The surgeon is able to identify the blue sentinel node(s) by direct visualisation, the radioactive sentinel node(s) using the handheld gamma probe, and then removes these sentinel node(s). If more than one sentinel node is found, all the sentinel nodes are removed.
It is very important to understand and remember that lymph nodes that are successfully ‘mapped’ (i.e. that show up on the nuclear medicine scan, hand held probe or blue dye tests) do not necessarily contain cancer cells. Rather, they are the first lymph nodes likely to be affected if cancer cells have escaped into the lymphatic system.
Does Sentinel Node Biopsy influence whether I have a Lumpectomy or a Mastectomy?
No – Having sentinel node biopsy will not affect whether your tumour is suitable for lumpectomy (wide local excision) or mastectomy.
When is sentinel node biopsy performed?
Sentinel node biopsy is usually done at the same time as breast surgery (lumpectomy or mastectomy) but sometimes it may be performed as a separate procedure. Jane O’Brien feels that it is often preferable, for example, to perform the sentinel node biopsy as a separate procedure before mastectomy when immediate reconstruction is desired. This allows for the final pathology of the sentinel nodes to be available, so that a completion axillary clearance can be performed at the time of mastectomy/reconstruction if sentinel nodes are positive. In addition, the need for post mastectomy radiation may be able to be predicted based on sentinel node status, which may influence reconstructive decision making. This is not a commonly used strategy, but one which Miss O’Brien finds particularly useful.
What is a false-negative result?
In a small number of women, the sentinel nodes do not have cancer cells, even though there are cancer cells in other lymph nodes in the armpit. This is called a “false-negative” result and it gives the patient and the doctor a false sense of security about the extent of cancer in the patient’s body. A meta-analysis of 69 trials with a total of 8,059 patients in whom SLNB was systematically followed by axillary dissection showed substantial variability in SLNB performance, with an average false negative rate (FNR) of 7.3% (range 0% to 29%).
False-negative SNB results may impair patient outcome for several reasons: missed nodes might lead to axillary recurrence that can be potentially difficult to treat on occasions, involved axillary nodes may be a potential secondary source of distant metastases, and understaging affects decisions about systemic therapy and specific radiation therapy fields to the breast, chest wall and nodal basins.
The FNR varies between different breast cancer treatment centres/surgeons, and false-negative results are much more frequent for inexperienced surgeons. The false-negative rates often quoted are approximately 5 to 10 percent, however quite alarmingly, recent multi institutional studies have actually revealed SLNB false-negative rates ranging from 5.5% to 16.7%, (SNAC 5.5%, Almanac 6.7%, NSABP-B32 9.8%, Sentinella/Givom 16.7%) which are much higher than the target (<5%) set by the 2005 guidelines of the American Society of Clinical Oncology.
Jane O’Brien regards the chance of a false negative result with SLNB, which effectively “understages” the patient, thereby increasing the risk of axillary recurrence and resulting in potential undertreatment, as a major concern , and in her opinion all possible attempts should be made to reduce to an absolute minimum the risk of a false negative result.
A false-negative result can occur because the lymphatic vessels running to the lymph nodes that have cancer cells in them are completely blocked by cancer cells. This means that the dye/radioactive material may enter other normal lymph nodes instead. To minimise the chance of a false-negative result caused by tumour blockage of lymphatic channels, the surgeon should always remove any enlarged/palpably abnormal feeling nodes that are found at the time of surgery, even if they are not radioactive or do not contain blue dye.

The greatest proportion of successful mappings and the lowest false-negative rates have been associated with studies in which both blue dye and radiolabelled colloid were used. In the Axillary Lymphatic Mapping Against Nodal Axillary Clearance (ALMANAC) validation study, the FNR was 6.7%. However, if only blue sentinel nodes are considered, the FNR was 9.1%. Likewise, the FNR would have been 10.9% based on isotope alone . In the Sentinella/GIVOM trial, blue dye was not used and the FNR was higher (16.7%) than in other trials. The preponderance of evidence also suggests that SLNB using blue dye as a single agent is not the optimal technique. Jane O’Brien always uses the dual technique, due to the evidence that the combined technique is more accurate, and is associated with a lower false negative rate. You should check with your surgeon how he/she performs sentinel node biopsy.
The SLN was originally defined as a single node, the first which directly receives lymph from the tumour, however experience gained with SLN biopsies, regardless of the technique used (blue dye, isotope, or both), has shown that multiple sentinel nodes are present in most breast cancer patients, and it is now a widely accepted concept that cancer cells often drain directly to a group of nodes rather than to a single node.
The number of SLNs obtained at operation is variable. The mean number of SLNs reported in studies in the literature ranges from 1.2 to 3.4 per patient. (McCarter et al, 2001)The number of SLNs that need to be removed for accurate lymph node staging is debated. Studies have suggested that removal of multiple SLNs provides for optimal detection of metastatic lymph node disease. Multiple studies, including the NSABP-B32 trial and the ALMANAC validation study have shown the influence of the number of resected nodes on the false-negative rate. The table below shows the false negative rates associated with the number of sentinel nodes removed in a study of over 4000 patients published in Archives of Surgery in 2007 (Chagpar et al).
False Negative Rate Associated with Number of Sentinel Nodes removed
|
No of SLN |
False NegativeRate (%) |
|
1 |
25.4 |
|
2 |
14.5 |
|
3 |
10.3 |
|
4 |
9.4 |
|
5 |
8.8 |
|
>5 |
7.7 |
A surgeon therefore must weigh the risk of missing a pathologically positive lymph node against the potential risks of SLND so extensive that the number of dissected lymph nodes essentially would equal that of a completion ALND, thereby potentially negating the benefits of SLND. Whether the removal of a few additional SLNs in the patient with multiple SLNs will worsen the morbidity of the procedure is unproven and in fact several studies suggest that it is not the case. Sener et al addressed this issue in a series of 303 patients who underwent SLNB alone and observed that the mean number of LNs removed was ‘‘similar’’ in both the lymphoedema and no-lymphoedema groups (Cancer, 2001). A Memorial Sloan Kettering study of 600 patients who underwent SLNB with a median follow-up of 5 years, found that 5% of patients had developed lymphoedema, but importantly there was no association between the number of LNs removed and the change in upper extremity measurements or in the incidence of lymphoedema. A median of 3 nodes (range 1–17) were removed during the SLNB. Factors associated with lymphoedema included weight and body mass index. (Ann Surg Oncol, 2010)
In SLNB, a “cherry-picking” technique is used for removal of the SLNs leaving the axillary lymphatics in areas away from the sentinel nodes intact, whereas in ALND, the axilla is dissected in an en bloc fashion, completely resecting the tissue in an anatomically defined area, including the entire axillary fat pad and any lymphatic vessels that are traversing the axilla from the upper extremity. It therefore may be that other factors, such as the global disruption of the lymphatic channels during axillary lymph node dissection, play a larger role in development of lymphoedema than does the number of lymph nodes removed.
There is also no evidence to suggest that it is possible to predict intraoperatively which of the sentinel nodes is most likely to contain tumour, ie it is not necessarily the hottest and/or most blue node. Camp et al, in 2004 demonstrated that in only 74% cases was the tumour bearing node the most radioactive ie in 26% of cases it was a lesser radioactive node. Jane O’Brien therefore feels very strongly that all hot or blue nodes should be resected, and that careful palpation by the surgeon of the operative field should also be performed to identify any suggestive large, hard non-blue and non-radioactive nodes, which should also be removed. This is because of the evidence, as outlined above, showing the influence of the number of resected nodes on the false-negative rate ie the number of SLNs removed is a powerful independent predictor of FNR and also the inability to predict which of multiple sentinel nodes, is the most likely to harbour tumour. She feels that risking a potential false negative rate of 25% by removing only a single sentinel node is unacceptable, and she searches very carefully for, and removes all sentinel nodes for pathological evaluation. If the possibility of a false negative SLNB result concerns you, check with your breast surgeon as to his/her personal SLNB philosophy/technique.











