Body Weight And Breast Surgery Complications
Body Weight And Breast Surgery Complications
Obesity is associated with a nearly 12-fold increased odds of postoperative complications after elective breast surgery.1 The complication rate is increased across all breast procedures in obese patients compared to ideal weight patients, however because the baseline complication rate is higher in more complex breast procedures, it is in association with more complex procedures that the impact of obesity is greatest. There is a progressive increase in the risk of complications with increasing levels of obesity (class 1, class 2 and class 3) compared to normal weight.
Patients should be made aware of their weight status category and it is important that breast surgeons and plastic surgeons make obese patients aware of the risk of the increased risk of post-operative complications, particularly when contemplating non-oncologically essential surgery, such as breast reconstruction, in addition to essential breast cancer surgery in the form of either lumpectomy or mastectomy. Patients need to realise that this is not a “fat shaming” or “victim blaming” exercise, but with almost two thirds (63%) of Australians now overweight or obese (36% overweight but not obese, and 28% obese), there has been a progressive “normalisation” of obesity to the extent that many overweight and obese people are unaware that they are overweight or obese, and therefore do not realise that the increase in post-operative complication applies to them. A British study of weight perception found self-identification of obesity to be low, with the proportion of obese adult women selecting the term ‘obese’ to describe their body size declining from a 13% in 2007 to an even lower level (11%) in 2012. A 2016 University of Sydney research similarly revealed that more than one in four (26.8%) overweight or obese Australians don’t realise they’re overweight or obese.
 Above: Post Mastectomy cellulitisComplication rates in breast cancer surgery overall are generally fairly low, with wound infection being the most common. In a multivariate analysis of 26,988 patients, a high body mass index and current tobacco use were the only independent risk factors for the development of a postoperative wound infection across all breast procedures in a multivariate analysis of 26,988 patients.2
Above: Post Mastectomy cellulitisComplication rates in breast cancer surgery overall are generally fairly low, with wound infection being the most common. In a multivariate analysis of 26,988 patients, a high body mass index and current tobacco use were the only independent risk factors for the development of a postoperative wound infection across all breast procedures in a multivariate analysis of 26,988 patients.2
There are potentially two aspects for the surgeon to assess in relation to the risk of surgical complications. The first is the baseline risk associated with the oncologically essential breast cancer surgery, whether it be lumpectomy or mastectomy. The second is the added risk of any potential additional non oncologically essential surgery such as breast reconstruction, contralateral prophylactic mastectomy (CPM/removal of the other breast for preventive purposes) or contralateral breast reduction.



In patients in whom it is possible based on preoperative core biopsy pathology to predict the need for chemotherapy (eg HER2 +ve and triple negative breast cancer) there are many potential advantages in administering preoperative (neoadjuvant) chemotherapy, one of which is that any surgical complications do not delay commencement of chemotherapy, as it has already been administered prior to surgery, and this option may therefore be particularly attractive in women in whom the risk of surgical complications is significantly elevated because of a high BMI. In addition, overall physical conditioning can potentially be optimised during chemotherapy prior to surgery by undertaking a supervised oncology prehabilitation programme.
With hormone receptor positive/HER2 negative breast cancer, which is the commonest breast cancer subtype, it is commonly not possible to definitively ascertain prior to surgery whether there will be a need for postoperative adjuvant chemotherapy, and post-operative wound complications, if prolonged, may potentially delay the commencement of chemotherapy. The oncological treatment must always take priority, and there are circumstances in which the treatment team may advise against performing other than oncologically essential surgery, because of an elevated risk of complications. A patient with a BMI over 40 for example who requires a mastectomy, may be advised that an immediate breast reconstruction is medically contraindicated, and that the preferred option in their case is to initially undergo only the oncologically essential surgery, followed by chemotherapy and radiotherapy as required, and then subsequent delayed breast reconstruction can be undertaken, preferably after some weight loss has been achieved.
A number of studies have demonstrated that obesity is associated with higher rates of surgical complications, including infection, seroma, and repeat operations, and is also linked to longer hospital stays. In a study of 2403 obese and 5597 non obese women undergoing breast surgery, the rate of overall complications, including infection, pain, delayed healing, implant removal, seroma, and haematoma, was 18.3% in obese women vs 2.2% in non obese women. The higher risk of complications was seen across procedure types.1 The overall complication rate is higher in more complex breast procedures, such as breast reconstruction, although is increased across all procedures in obese patients compared to ideal weight patients. A study of 7207 women undergoing mastectomy without reconstruction, showed that major and minor complications increased as BMI increased.3 (Fig below)
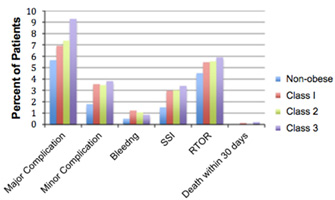 Percent of patients with complications after mastectomy (without reconstruction) based on BMI3
Percent of patients with complications after mastectomy (without reconstruction) based on BMI3
A larger trial that included 55,903 patients with breast cancer confirms these findings; obese vs nonobese individuals had higher rates of overall complications (9.0% vs 5.9% for lumpectomy; and 5.9% vs 4.8% for mastectomy; leading to longer hospital stays and higher costs.4
Another large study utilizing the National Surgical Quality Improvement Program data set, which included 15,937 women who underwent breast reconstruction, evaluated 30-day complication rates for those with a BMI of at least 40 vs those with a BMI of less than 30. Researchers demonstrated an increased risk of wound complications, return to the operating room, and surgical site infection in obese women, as well as longer operative times.5 A smaller study of 551 patients undergoing breast reconstruction with implants had similar findings, with overall complication rates of 9.9% in normal-weight women, 23.3% in overweight women, and 20.6% in obese women. Additionally, BMI was found to be an independent and strong predictor of flap necrosis, infection, and seroma.6
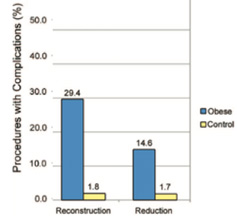 Above: Presence of any complication in the 30-day postoperative period after breast surgery, by procedure type 1
Above: Presence of any complication in the 30-day postoperative period after breast surgery, by procedure type 1
Breast reconstruction for obese patients is a challenging task. It is well known that obesity has adverse effects on postoperative outcomes, and a similar phenomenon has been reported in the field of breast reconstruction. In particular, prosthesis-based reconstruction for obese patients shows high reconstruction failure rates and catastrophic outcomes, and therefore autologous tissue flap reconstruction has been preferred for obese patients. Among various options in autologous reconstruction, abdominal flaps are widely used because they provide not only abundant soft tissue for reconstructing large and ptotic (saggy) breasts, which are common in obese patients, but also acceptable abdominal donor site morbidity.
Breast reconstruction surgeries are associated with high rates of postoperative complications, ranging from 43 to 64%, and in one report, almost two thirds of women undergoing bilateral prophylactic mastectomy had at least one complication after surgery, and fewer complications were observed in women who did not undergo reconstruction. Numerous studies have shown that increasing BMI is strongly correlated to an increase in postoperative complications for breast reconstruction. One study found that obese patients can have as much as an 11.8-fold increase in the odds of experiencing a complication. Furthermore, each 1-unit increase in BMI can add 5.9% to a patient’s overall complication risk. A possible explanation for why obese patients are at higher risk for complications is that they have more breast surface area, and thus, the possibility for poor perfusion ultimately resulting in necrosis and infection is higher. In addition, the surgery for obese patients is often longer, which increases the potential for contamination. Whilst a progressive increase in post-operative complication rates have been demonstrated for BMIs above the ideal weight range, (25 and above), it is in the obese category (BMI 30 and above) that the increased risks become clinically relevant. There is no specific BMI cut off level above which immediate reconstruction is medically contraindicated, and other comorbidities such as smoking and diabetes are obviously taken in to account. However, with BMI levels of 37 and above, the risk of post-operative complications reaches a level where the alternative option of simple mastectomy, without immediate reconstruction, with a view to delayed reconstruction after cancer therapies are completed, needs to be seriously considered, ideally after the patient has undergone a medically supervised weight loss programme.11



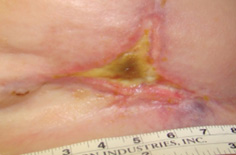
When immediate reconstruction is performed at the time of mastectomy, the native skin envelope is preserved (skin-sparing mastectomy/SSM) often including the nipple (nipple- sparing mastectomy/NSM), and thus the only challenge for reconstruction is to restore the breast’s volume and contour either by implant-based or autologous tissue flap methods. One of the complications of both SSM and NSM is mastectomy skin flap necrosis, which occurs after a mastectomy is performed when the overlying breast skin does not have enough blood supply to survive, and post operatively, the skin progressively becomes darker and necrotic and forms an eschar (dry scar).
Mastectomy skin flap necrosis is a relatively common problem after SSM and NSM mastectomy with immediate reconstruction. Review of the literature suggests the rate of skin flap necrosis after reconstruction to be around 15.8%, and some reports even cite rates as high as 30% if partial skin necrosis/desquamation is grouped in this category. It is important to identify which patients are most susceptible to skin flap necrosis. A review of the literature highlights numerous studies showing that a body mass index (BMI) over 30, higher mastectomy weight, active smoking, a history of preoperative radiation therapy, incision type and age over 65 years are significant factors.
Increased BMI is an independent risk factor for skin flap complications, with morbidly obese patients experiencing substantially more risk than their normal, overweight, and obese counterparts. Mastectomy weight is also a strong risk factor for flap necrosis, with increasing weight correlating with higher risk of necrosis. Patients with larger breasts, have increased complications, and higher mastectomy weight has been shown to be associated with greater body mass index. Large breast size yields a larger mastectomy flap surface area that may be more susceptible to impaired perfusion and ischaemic sequelae.
Below: Post-Mastectomy Skin Flap Necrosis. Left-Skin-Sparing Mastectomy (SSM) Right: Nipple-Sparing Mastectomy (NSM) (Note: As always, clinical photographs are NOT my own patients)


Patients with larger breasts often benefit from a Wise pattern skin reduction incisions (above left), as they frequently require reduction of the skin envelope, and these incisions are associated with an increased risk of mastectomy skin flap necrosis.
Following SSM and NSM, mastectomy skin flap perfusion is provided by means of vasculature in the subdermal and subcutaneous tissues. SSM and NSM in patients with larger breasts yields mastectomy flaps with a greater surface area and greater overall risk of of impaired perfusion to these flaps. The distance from the perforating vessels supplying these subdermal and subcutaneous plexuses to the nipple-areolar complex and edges of the mastectomy flaps is also inherently greater with increased breast size and therefore there is a progressively increased risk of ischaemic complications with larger breast size and higher mastectomy weight.
Obesity is a proven risk factor for numerous complications in abdominally based autologous breast reconstruction such as the currently commonly performed DIEP flap. As body mass index (BMI) increases, there is a proportional increase in complication rates. A recent meta-analysis of more than 6000 patients found significantly increased risk of almost all complications in obese patients including overall complications, recipient site complications overall, donor site complications overall, donor site wound infection, donor site seroma, mastectomy skin flap necrosis, recipient site delayed wound healing, and partial flap failure. Overall, the pooled incidence of total flap loss in obese patients was approximately 1.9 times higher than that in nonobese patients, but was still very low. (1.5% vs 0.8%). The rate of partial flap loss in obese patients was 2.6% and almost 3 times higher than that in nonobese patients (0.9%). The incidence of any flap loss was 2.1 times higher in obese patients than in nonobese patients (4.5% vs 2.1%).
The rate of overall abdominal complications was approximately 1.7 times higher in obese patients (19.2%) than in nonobese patients (11.5%) Although complications were higher in the obese group when compared with patients with normal BMI, alloplastic (implant based) reconstructions were associated with an even higher complication rate. Despite the elevated risk of complications in obese patients undergoing autologous reconstruction, satisfaction is significantly higher than that in patients undergoing implant based reconstruction.7
Findings were similar in a 2018 systematic review and meta-analysis which included 71,368 patients, 20,061 of whom were obese. Obese women (body mass index > 30 kg/m2) were 2.29 times more likely to experience surgical complications, 2.89 times more likely to have medical complications and had a 1.91 times higher risk of reoperation. The most common complication, wound dehiscence, was 2.51 times more likely in obese women.8
Obese patients exhibit higher rates of comorbidities, require longer operative times and inpatient stays, possess greater anaesthetic risk, and overall experience higher rates of morbidity, both medical and surgical, when undergoing breast reconstruction, and obesity is an independently associated risk factor for both medical and surgical complications.
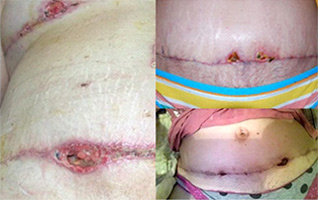
Breast reduction is often performed in conjunction with breast conserving surgery for cancer, and also as a symmetrisation procedure on the unaffected breast in women undergoing unilateral mastectomy with reconstruction. Postoperative complications are relatively common after breast reduction, with an incidence of 14%-53% in reported studies, and a 2016 meta-analysis found that increased BMI was the strongest predictor of complications including infection and wound dehiscence.9 Another meta-analysis found the pooled risk of skin and fat necrosis was 2.01 in the obese group (compared with the non-obese group). Tissue necrosis complications are relatively difficult to manage and frequently require additional surgical revision.10

 Above-typical examples of the type of wound complications common in obese patients following breast reduction surgery
Above-typical examples of the type of wound complications common in obese patients following breast reduction surgery
Several studies have shown that abdominal donor-site morbidity is higher in obese patients undergoing flap-based reconstruction with two studies reporting abdominal complication rates of 50% in obese patients.7 Studies have previously demonstrated that wound healing may be impaired in the obese due to decreased myofibroblast activity and deranged collagen maturation. These two altered processes represent critically important steps involved in the healing of a large donor- site wound and may likely predispose obese patients to delayed wound healing, especially the abdominal donor site wound.
Excessive subcutaneous fat tissue predisposes obese patients to impaired healing due to low regional perfusion and oxygen tension. Secondly there is an increase in operation time for the obese and a longer operation time has been described as a significant predictor of postoperative wound infections. Operations on obese patients take longer, the operating fields are deeper, the spaces in which an infection can set in are often greater and blood flow in fat tissue is less than in other types of tissue, which results in slower healing.
 Above: Abdominal donor site wound fat necrosisFat necrosis can occur after any surgery that removes and/or rearranges fat, and occurs when the blood supply to the fat is inadequate. It occurs most frequently in overweight/obese patients who have a thick layer of fat. The fat cells die, and as they die they release fatty acids and other chemicals that causes inflammation and swelling and sometimes pain. Usually fat necrosis presents as a non-tender lump, but can look a lot like a wound infection to the patient. It occurs most frequently in overweight /obese patients who have a thick layer of fat. In most cases the lump shrinks over time, and ends up as a firm little lump that usually does not require reoperation, but if it is a bother, the lump can be excised.
Above: Abdominal donor site wound fat necrosisFat necrosis can occur after any surgery that removes and/or rearranges fat, and occurs when the blood supply to the fat is inadequate. It occurs most frequently in overweight/obese patients who have a thick layer of fat. The fat cells die, and as they die they release fatty acids and other chemicals that causes inflammation and swelling and sometimes pain. Usually fat necrosis presents as a non-tender lump, but can look a lot like a wound infection to the patient. It occurs most frequently in overweight /obese patients who have a thick layer of fat. In most cases the lump shrinks over time, and ends up as a firm little lump that usually does not require reoperation, but if it is a bother, the lump can be excised.
Women with a BMI over 30 who develop abdominal donor site or breast reduction wound complications in the form of dehiscence, necrosis, infection or delayed healing are often a) unaware that they are obese, and/or b) not aware that obesity is the likely explanation for their wound problem. Their wounds are slow to heal, not because the plastic surgeon didn’t close the abdominal wound securely enough, or took the surgical drain out too early, but because excessive subcutaneous fat tissue predisposes obese patients to impaired wound healing due to low regional perfusion and oxygen tension and decreased myofibroblast activity and deranged collagen maturation.
The photos below demonstrate typical slow healing/wound dehiscence of abdominal donor site wounds in overweight subjects, and also in the photo on the left, delayed healing of the T intersection of a breast reduction wound.

In contrast to the wounds above, the photos below show typical abdominal donor site wounds in patients with a BMI in the ideal weight range. Despite the fact that the abdominal wound needs to be closed under greater tension in thinner subjects, wound problems are much less common.



The majority of surgical complications following breast surgery are relatively minor in nature and usually fairly easily dealt with, although a return to the operating theatre for wound debridement may be required. Sometimes reoperation is undertaken to debride a wound which would gradually heal over under normal circumstances, however in patients due to commence chemotherapy (normally started around 4 weeks after surgery) there may a desire to accelerate closure of the wound. In the absence of other significant risk factors such as diabetes or smoking, being overweight/obese is not commonly an absolute contraindication to proceeding with elective breast surgery such as reconstruction or breast reduction in addition to oncologically essential breast cancer surgery, however women whose weight is above the ideal weight range need to be made aware that their weight places them at a significantly elevated risk of wound complications, particularly if their BMI is 30 or above.
Obese patients exhibit higher rates of comorbidities, require longer operative times and inpatient stays, possess greater anaesthetic risk, and overall experience higher rates of morbidity, both medical and surgical, when undergoing breast surgery. Neglecting the risks of a high baseline BMI interferes with the surgeon’s ability to assess the risk of surgery and provide accurate information to the patient. It is very important that you are made aware of your body weight status prior to any breast surgery, especially if it is in the obese range (BMI>30) in which the risk of complications is significantly elevated, so that you are able to weigh up the potential risks and benefits of undergoing any non-oncologically essential surgery at the time of your breast cancer surgery, such as breast reconstruction or breast reduction, prior to proceeding.
Patients supply height and weight information on their patient registration form, and this is used to calculate BMI.
References:
- The Impact of Obesity on Breast Surgery Complications, Chen et al, Plastic and Reconstructive Surgery, 2011.
- High Body Mass Index and Smoking Predict Morbidity in Breast Cancer Surgery, de Blacam et al, Annals of Surgery, 2012.
- The impact of obesity on outcomes for patients undergoing mastectomy, Garland et al, Breast Cancer Research and Treatment, 2018.
- Attributable cost of obesity in breast surgery: a matched cohort analysis, Sun et al, American Journal of Surgery, 2015 .
- Impact of Obesity on Outcomes in Breast Reconstruction: Analysis of 15,937 Patients from the ACS-NSQIP Datasets, Fischer et al, Plastic and Reconstructive Surgery, 2013 .
- Body Mass Index as a Continuous Predictor of Outcomes After Expander-Implant Breast Reconstruction, Nguyen et al, Annals of Plastic Surgery, 2014.
- Effects of Obesity on Postoperative Complications After Breast Reconstruction Using Free Muscle-Sparing Transverse Rectus Abdominis Myocutaneous, Deep Inferior Epigastric Perforator, and Superficial Inferior Epigastric Artery Flap. A Systematic Review and Meta-analysis, Lee et al, Annals of Plastic Surgery, 2016.
- Impact of Obesity on Outcomes in Breast Reconstruction: A Systematic Review and Meta-Analysis, Panayi et al, Journal of Reconstructive Microsurgery, 2018.
- Risk Factors for Complications after Reduction Mammoplasty: A Meta-Analysis. Zhang et al, PLoS, 2016.
- Relationship Between Obesity and Surgical Complications After Reduction Mammaplasty: A Systematic Literature Review and Meta-Analysis, Myung et al, Aesthetic Surgery Journal, 2017.
- The Advantages of Free Abdominal-Based Flaps over Implants for Breast Reconstruction in Obese Patients, Garvey et al, Plastic and Reconstructive Surgery, 2012
You will need the Adobe Reader to view and print these documents.![]()











