Prepectoral Implant Based Reconstruction
![]() Prepectoral Implant-Based Breast Reconstruction: a Joint Consensus Guide
Prepectoral Implant-Based Breast Reconstruction: a Joint Consensus Guide
![]() Prepectoral Implant Based Breast Reconstruction
Prepectoral Implant Based Breast Reconstruction
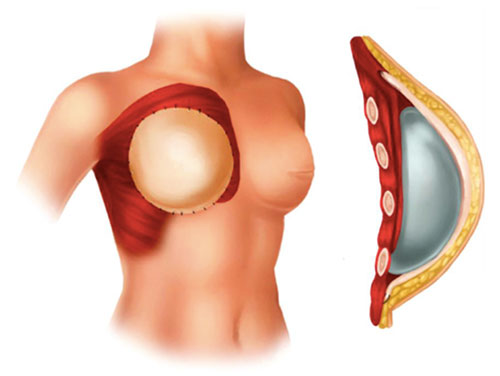
Breast reconstruction with a “prepectoral” prosthesis wrapped in ADM (acellular dermal matrix) is the newest type of implant-based breast reconstruction (IBBR). The prepectoral approach can be used in conjunction with either single stage direct-to-implant (DTI) reconstruction or two stage tissue expander reconstruction. Prepectoral reconstruction is an alternative to the more common “subpectoral” and “dual-plane” approaches. (Autologous tissue flap reconstructions such as DIEP flaps are routinely placed prepectorally)
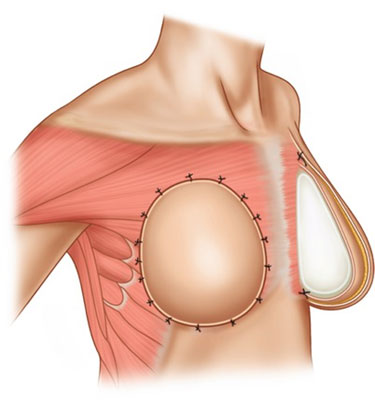 Prepectoral Implant positioned in front of chest wall muscle
Prepectoral Implant positioned in front of chest wall muscle
One problem with implant-based breast reconstruction is that many women experience pain and chest tightness. The pectoralis muscle is designed to be flat against the chest wall. When a breast implant is placed under the pectoralis muscle, it can be uncomfortable and many women never escape the discomfort as long as the implants remain. Furthermore, when the woman flexes her chest muscle, there is a hyper-animation deformity in which the pectoralis muscle pushes down on and deforms the implant, causing it to move up and down in an odd way. Finally, the constant action of the pectoralis muscle pushes the breast implants into the armpits so that over time the breasts migrate wider apart. In recent years, however, it has become possible to place breast implants over the muscle for breast reconstruction to give women a more comfortable and natural result.

Traditionally, implants were placed under the pectoralis muscle because the tissue left behind by the mastectomy was thin and there was a risk that the implant would erode through the skin. The rationale was that by placing an implant underneath the pectoralis muscle, there was an extra layer of tissue between the implant and the outside world to prevent the implant from becoming exposed. If the implant did erode through the skin, it was considered infected, and would require removal. The risk of complications was even higher for patients who underwent radiation, since radiation damage makes the skin less elastic and more difficult to heal. In fact, radiation treatment has long been considered a relative contraindication for breast reconstruction with implants.

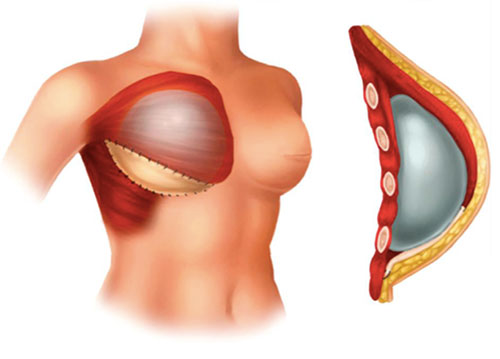
Placing the breast implant over the muscle and directly under the skin – prepectoral breast implant placement – is anatomically correct, as the anatomic position of actual breast tissue before mastectomy is over the pectoralis muscle and under the skin. Since the pectoralis muscle ordinarily lays flat against the chest wall, placing the breast implant under the pectoralis muscle – or subpectoral breast implant placement – is unnatural and uncomfortable. When a foreign body is placed underneath the pectoralis muscle, it is like having a stone in a tight shoe that you cannot remove. When a breast implant is placed over the muscle in the prepectoral position, the implant is anatomically positioned in the same spot where the breast tissue used to be. The result is much more natural and comfortable, and since the implant is over the muscle the action of the pectoralis muscle does not force the implant into the armpits.
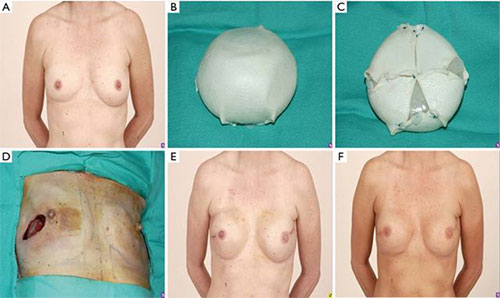 Example of prepectoral reconstruction with complete wrapping of prosthesis in ADM (A) Pre-operative; (B,C) preparation ofprosthesis; (D) Intra-operative (E,F) Post-operative
Example of prepectoral reconstruction with complete wrapping of prosthesis in ADM (A) Pre-operative; (B,C) preparation ofprosthesis; (D) Intra-operative (E,F) Post-operative
One concern with placing breast implants over the muscle is that the pectoralis muscle is not providing an extra layer of tissue over the implant. To make up for this, surgeons use acellular dermal matrix (ADM) to provide an additional barrier between the implant, the skin, and the outside world. Harvested from the dermal layer of human skin, ADM has been stripped of reactive cell components but retains the strength and flexibility of skin due to the biologic qualities and structure of natural collagen. Not only does the ADM provide an extra layer of soft tissue coverage over the implant to prevent exposure, but it can also soften the edges of the implant itself so that the outlines of the implant are not visible through the skin. The use of ADM may slightly increase the risk of infection and seroma formation, but it has been used in conjunction with dual plane reconstruction for years and is considered the standard of care. Prepectoral breast implants require more ADM than subpectoral breast implants, so the risk of infection and seroma formation may be slightly higher. One advantage to ADM is that it eventually integrates into the body and develops a blood supply. Once this occurs, it is incorporated by the body and is less likely to develop infection or other problems. ADM is also believed to reduce the risk of capsular contracture.

Breast reconstruction with prepectoral implants wrapped in ADM is a significant advance in implant-based breast reconstruction. While natural tissue breast reconstruction may have fewer problems over the long term, prepectoral implant breast reconstruction is a good option for women who are unable or unwilling to undergo breast reconstruction with their own tissue. The use of ADM may theoretically increase the risk of infection and seroma in prepectoral breast reconstruction when compared to subpectoral breast reconstruction, but the underlying issue in both prepectoral and subpectoral implant-based breast reconstruction is that implants and ADM are foreign bodies, and any type of implant-based breast reconstruction will inherently have higher risk of complications over a lifetime when compared to natural tissue breast reconstruction. If a woman is committed to undergoing breast reconstruction with implants, however, placing breast implants over the muscle in prepectoral breast reconstruction may offer a natural and comfortable outcome.
Appropriate patient selection is critical for a successful outcome in all forms of breast reconstruction, and is critical consideration when employing this new technique.
Prepectoral reconstruction is not widely available in Australia, and Jane O’Brien’s team is one of less than half a dozen in Victoria who are currently offering our patients the option of prepectoral reconstruction.
In 2018 in Jane O’Brien’s practice,
- 38% implant based reconstructions at the time of mastectomy for breast cancer were prepectoral (with ADM)
- 50% of patients undergoing bilateral risk reduction mastectomy with implant based recon underwent prepectoral direct-to-implant (DTI) reconstruction with ADM.
 Jane O’Brien with plastic surgical colleague Edmund Ek
Jane O’Brien with plastic surgical colleague Edmund Ek
What is “prepectoral” breast reconstruction?
“Prepectoral” breast reconstruction is a form of implant based reconstruction in which the breast prosthesis (either a tissue expander or a permanent implant) is placed in front of the pectoral (chest wall) muscle, rather than behind it.
The pectoral muscle doesn’t have to be lifted which lessens pain. When the implant is on top instead of under the muscle, there is no “animation” deformity and this makes exercising and wearing form-fitting clothes much easier.
Animation Deformity
Animation deformity, which can occur in the setting of submuscular or dual plane implants, is the unnatural movement of the breast when the pectoral muscle is activated. It occurs with any movement of the pectoralis major muscle, and results in visible contraction and displacement of the breast. The unnatural movement wrinkles the skin and pushes the implant down and outward.
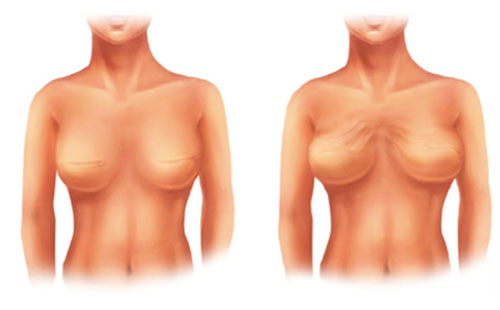
 Animation deformity with contraction of pectoralis muscle
Animation deformity with contraction of pectoralis muscle

Click here to watch full video:
Further example of animation deformity – click here
3 Benefits of Pre-Pectoral Reconstruction
- The patient experiences less pain compared to implants placement under the chest muscle.
- Movement and contraction of the chest muscle will not affect the implant and therefore limits animation deformity.
- A more natural-appearing, shaped breast can be achieved with this method.
Ideal candidates for Prepectoral Reconstruction:
Patients with minimal comorbidities, an active lifestyle, small- to medium-sized breasts, and good intraoperative tissue perfusion are good candidates for this surgery.
- Patients with a low body mass index (BMI) (< 35 kg/m2),
- Non- or ex-smokers,
- Grade 1 or 2 ptosis (ie breasts that are not very saggy)
- Anticipated breast volume of resection less than 500g
Patient lifestyle should be taken into consideration, particularly athletes who require extensive pectoralis major use and require preserve shoulder functionality.
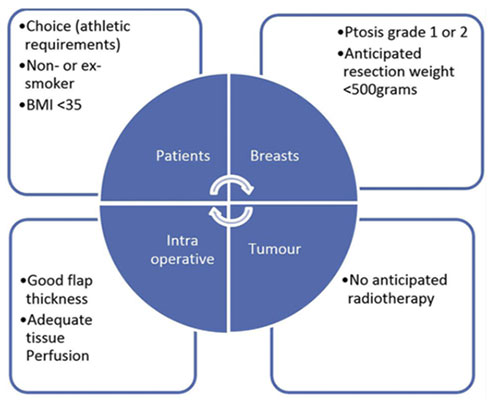 Patient Selection Criteria
Patient Selection Criteria
The main patient benefits of the prepectoral approach include elimination of animation deformity and the comfort derived from leaving the pectoralis chest wall muscle undisturbed. The elevation, disinsertion, and stretching of the pectoralis major muscle, and in some cases the serratus anterior muscle, are associated with the potential for increased clinical side effects.
These include greater risk of animation deformity and increased loss of strength. Immediate prepectoral breast reconstruction, with placement of the prosthesis above the pectoralis muscle, might reduce the incidence of these clinical morbidities. The elimination of muscle dissection makes the immediate postsurgical recovery period easier for patients to tolerate. With prepectoral breast reconstruction, it is possible that patients may exhibit less overall discomfort associated with surgical recovery, relative to submuscular reconstruction, because of the elimination of pectoralis major muscle dissection, disinsertion, and stretching.
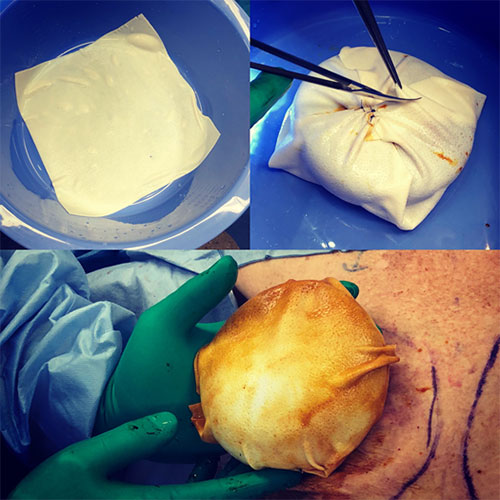 Intraoperative photo of ADM (top left) and implant wrapped in ADM (top right and bottom)
Intraoperative photo of ADM (top left) and implant wrapped in ADM (top right and bottom)
Leaving the muscle in its native position allows for a procedure that is less invasive and better tolerated by patients than its submuscular counterparts. There is comparatively less pain, with a decreased need for post-operative narcotic analgesia, faster recovery, elimination of animation deformity, improved long-term comfort as well as a more natural appearing breast.
These advantages arise from the fact that the reconstructed breast takes the place of the excised one, without any additional disruption to the natural anatomy. It is associated with a lower rate of shoulder dysfunction, and also a lower incidence of capsular contracture.
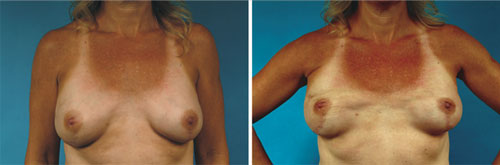
Rippling:
In prepectoral breast reconstruction, the pectoralis major muscle is not available to provide an additional layer of soft tissue coverage over the upper pole of the implant. The thinner flaps provide less fullness in the upper pole of the breast and do less to camouflage the edges of the implant or wrinkles in the outer shell that manifest themselves as skin rippling or contour irregularities.
One potential risk of prepectoral breast reconstruction therefore is a higher rate of visible “rippling” over the permanent implants, given the thinner upper pole coverage, compared with submuscular/dual plane reconstruction. Rippling refers to visible folds on the surface of the breast, transmitted from an underlying breast implant, and is typically most apparent in the upper inner portions of the breast. Rippling may require further intervention such as lipomodeling.
 Rippling visible only when patient leans forward
Rippling visible only when patient leans forward
 Rippling visible with the patient the upright
Rippling visible with the patient the upright
Decreased soft tissue coverage in the pre-pectoral plane is less effective in disguising implant rippling or camouflaging the edges of the implant particularly in the upper pole of thin women. Without submuscular or partial subpectoral placement of the implant, there may be a clear “step-off” visible between the chest wall and the prepectoral implant. The primary means for correcting these deformities is autologous fat grafting.
Prepectoral implant reconstruction (left), demonstrating “rippling” deformity. Fat grafting to upper pole (right) corrects defect.
Background:
Prepectoral implant placement is not a new concept, and with the introduction of prosthetic (implant) breast reconstruction in the 1960s, the primary method of reconstruction was the subcutaneous, prepectoral placement of a tissue expander or permanent implant. This was still the reconstructive method of choice when I arrived at the Nottingham Breast Unit in 1997. The complications associated with subcutaneous prepectoral placement however included high rates of skin flap necrosis and capsular contracture, leading to removal of the implant. These complications were largely due to a lack of soft-tissue support for the implanted prosthesis. Due to the high rate of complications, surgeons over time switched to placing tissue expanders and implants in the subpectoral space, under the chest wall muscle, with coverage by the pectoralis major and serratus anterior, and the use of a total submuscular pocket for prosthesis coverage, to prevent wound dehiscence and implant exposure has been the preferred choice until recently.

Total submuscular reconstruction is almost invariably undertaken in two stages with initial placement of a tissue expander at the time of mastectomy, followed by subsequent serial expansion of the subpectoral space and the exchange of the tissue expander for a permanent implant at a second operation.
The field of implant-based breast reconstruction has been radically changed since the recent introduction of meshes, resulting in the adoption of new techniques, and over the past decade, the introduction of meshes has revolutionized breast reconstruction. A wide variety of biological and synthetic meshes are available.
biological mesh, referred to as an acellular dermal matrix (ADM), is a scaffold of dermis from either cadaveric human (eg FlexHD, Alloderm, Allomax), porcine, bovine, or bovine pericardial tissue. They are made devoid of their cell content and sterilized, and as such, they are considered to be noninflammatory. The biological scaffold allows rapid host revascularization and cell repopulation, facilitating a good surgical outcome.
Synthetic matrices are also being used in breast reconstruction as an alternative to ADMs. These are made from plastic-like material: absorbable (Vicryl), long-term absorbable (TIGR), or non- absorbable titanium-coated polypropylene mesh (TiLOOP).

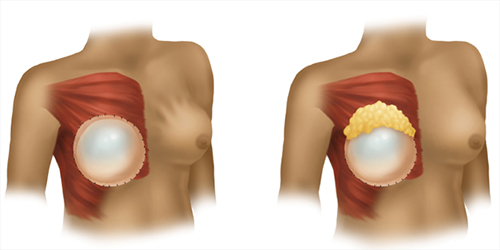
The morbidity associated with subpectoral implants, along with the advent of the use of ADMs, led to a partial muscle coverage approach, known as the dual-plane approach, which facilitated single stage direct-to-implant reconstruction (DTI). Now, with the wider adoption of ADM and autologous fat grafting, are considering the prepectoral approach is being reconsidered.
 Dual-plane Reconstruction- Partial muscle overage + ADM approach: the pectoralis muscle reinforces the upper pole and ADM reinforces the lower pole
Dual-plane Reconstruction- Partial muscle overage + ADM approach: the pectoralis muscle reinforces the upper pole and ADM reinforces the lower pole
Unfortunately, subpectoral and dual plane prosthesis placement is associated with its own set of complications. High levels of postoperative muscle elevation pain, muscle animation deformity, muscle spasms, and “windowshading,” along with a decrease in strength and mobility, resulted in unfavorable views of this reconstructive approach. Windowshading is the creasing of overlying skin when the underlying muscle contracts, usually occurring when a scar forms between muscle edge and surrounding soft tissue. Both animation deformity and windowshading are based upon the tissue expander or implant being placed below the pectoralis muscle.
Over time, the chest wall can also develop a concavity secondary to the constant muscle contraction and placement of the prosthetic device on the chest wall.
Potential benefits of a prepectoral approach include the elimination of the pain and morbidity from muscle elevation as well as the muscle animation deformity, as the need for muscular manipulation is obviated with a subcutaneous implant insertion. Furthermore, recovery time is shortened and surgeons often have greater control of the shape and form of the breast reconstruction. Since there is no overlying muscle to compress the implant, there is less of a chance for implant malposition. Importantly, patients notice improved mobility and do not have to deal with decreased muscle strength. As such, prepectoral breast reconstruction is a suitable technique for the ideal candidate.
 Wrapping of prosthesis in ADM
Wrapping of prosthesis in ADM
As with any procedure, proper patient selection is imperative for ensuring a successful outcome. Optimal patient selection is one that is non-diabetic and non-smoking with a body mass index (BMI) < 35 and well-perfused mastectomy skin flaps. Well-vascularized flaps are critical to achieve success with this procedure. Prepectoral breast reconstruction may also be a viable option for patients who present with a need for a revision of a previous submuscular or dual-plane reconstruction, who experience muscle animation deformity or pain. Relative contraindications to prepectoral reconstruction include a history of radiation, smoking, high BMI, large, pendulous breasts and poor tissue quality. Patients at high risk for mastectomy flap necrosis are those with a high BMI, smokers, or diabetics. Like dual plane reconstruction, prepectoral implant-based reconstruction can be performed as either a one stage (DTI) or two stage procedure. In the 2-stage process, the first stage involves the insertion of a tissue expander and the second stage is when the expander is exchanged for a permanent breast implant.
 Prepectoral approach: Implant is placed in the subcutaneous, prepectoral plane. ADM provides overlying reinforcement
Prepectoral approach: Implant is placed in the subcutaneous, prepectoral plane. ADM provides overlying reinforcement
Following a skin or nipple-sparing mastectomy, the prosthesis is placed in the prepectoral space, in place of the removed breast. If pressure on the skin flaps is possible, then a tissue expander can be used. The implant is placed under-filled, ensuring that there is no increased pressure to the flaps and expanded at a later date once viability of the flaps is confirmed.
The ADM is then sutured over the prosthesis (tissue expander or implant) The use of ADM is helpful in achieving a successful re- constructive result. Serving as a cover and soft-tissue reinforcement for the implant, it has been demonstrated to decrease rates of capsular contracture by reducing inflammation. The entire anterior (front) surface of the prosthesis is covered with ADM, with variable portions of the posterior (back) surface covered as well.
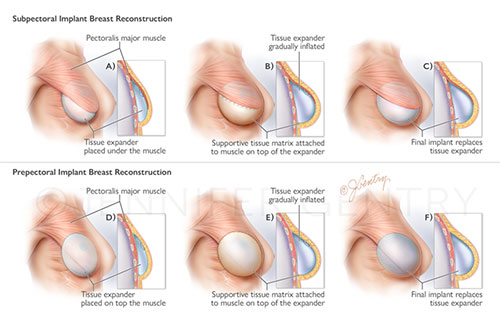 Tissue Expander Reconstruction. Top: Subpectoral/dual plane with ADM. Bottom: Prepectoral with ADM
Tissue Expander Reconstruction. Top: Subpectoral/dual plane with ADM. Bottom: Prepectoral with ADM
Autologous fat grafting is also a useful adjunct to performing the prepectoral technique. This procedure aids in filling in any volume deficits in the upper pole of the breast that may be present after placement of implant and ADM. Using this technique helps eliminate potential rippling that can occur with prepectoral implant placement.
Frequently Asked Questions
Should I consider prepectoral Implant reconstruction?
If you lead a very active lifestyle, there are potential benefits in not disturbing your pectoral muscle. The benefits are potentially less pain, both immediately post-op and long term, and ideally a more natural appearing breast with no animation deformity, compared to the more traditional method of placing the implant under the muscle.
Would prepectoral reconstruction be an appropriate option for me to consider?
If you choose to undergo implant-based breast reconstruction, the pre-pectoral method may be an option for you. Prepectoral reconstruction is most suitable for women who are within a healthy weight range, ideally with a BMI less than 30, have breasts that are not overly large or saggy, are non-diabetic, non-smokers and have not had previous radiotherapy.
How is pre-pectoral Implant reconstruction different from traditional implant reconstruction?
Traditional implant reconstruction places the implant behind the chest muscles. This requires surgically separating the chest muscle from the underlying chest wall. Commonly, an acellular dermal matrix is used as a sling to help support and cover the lower part of the implant. Prepectoral reconstruction places the implant in front of the chest wall muscles. As a result, the chest muscles remain in their normal position, and continue to function normally. In addition, in prepectoral reconstruction, the chest muscles are not stretched out during expansion, potentially making the process less painful.
What is an acellular dermal matrix?
An acellular dermal matrix (ADM) is an engineered sheet of tissue made from cadaver skin. Cells are removed from the tissue allowing your cells and blood vessels to grow into the matrix. This process will allow the acellular dermal matrix to incorporate and eventually become a part of your body.
Can pre-pectoral breast reconstruction be done direct to implant (DTI), without using a tissue expander?
It is possible to place either an implant under the skin, in front of the chest muscles, bypassing the tissue expander step. The skin overlying the implant after mastectomy must be in good condition, and a smaller breast implant may be chosen to decrease the stress on the overlying skin. If you are undergoing prepectoral reconstruction, and wish to “upsize”, a two stage procedure, with initial tissue expansion is required.

What if I require post-mastectomy radiotherapy (PMRT)?
Autologous tissue flap reconstruction is usually a better reconstructive option for women who require, or are highly likely to require, post-mastectomy radiotherapy, however not all women are suitable for, or desire, autologous reconstruction. Several studies have shown the beneficial effect of biological ADMs on the capsular contracture rate after implant-based breast reconstruction, and there is now evidence in the litearature suggesting that prepectoral implant based reconstructions tolerate radiotherapy better than subpectoral. An American study published in 2018 (Sinnott et al, Annals of Surgical Oncology) found that patients undergoing subpectoral breast reconstruction who received PMRT had a capsular contracture rate three times greater, with more severe contractures, than the patients receiving PMRT who underwent prepectoral breast reconstruction. Based on the current evidence, if you are undergoing implant based reconstruction, and require post mastectomy radiotherapy, and you are a suitable candidate, prepectoral reonstruction may be a better option for you than subpectoral.
What about cost?
Prepectoral reconstruction is associated with a significantly higher cost than other implant based reconstructions. The additional cost is due to the much greater volume of ADM required to cover the prepectoral implant, compared to dual-plane reconstruction. The biological mesh products, particularly those using human cadaveric skin, require extensive pretreatment, and as such are very expensive to produce. Some biological ADMs eg FlexHD, are covered by private health insurance, but are generally out of the financial reach of self-funders, and are not available in public hospitals, although some public hospitals may offer some of the more affordable synthetic mesh products.
Is prepectoral reconstruction widely available?
Prepectoral reconstruction is not widely available in Australia, and Jane O’Brien’s team is one of less than half a dozen in Victoria currently offering the option of prepectoral reconstruction to our patients.

Jane O’Brien (above left) and plastic surgeon Ed Ek (above right) operating simultaneously, performing immediate bilateral prepectoral direct-to-implant (DTI) reconstruction with Flex HD ADM at the time of bilateral nipple-sparing mastectomy (NSM).











